I have received a number of inquiries from both customers and colleagues on the topic of meaningful use (MU) audits. As part of the program, CMS is required to audit a sample of both hospitals and eligible professionals participating in the program. The word “audit” can elicit a visceral response for some when used in the context of CMS. Today, let’s take a look at what we know and attempt to ease the pain.
Background
MU audits have been in place since the Summer of 2012. Beginning with attestations submitted in January 2012, CMS began to perform prepayment audits in addition to the standard post-payment audit. CMS has contracted with a CPA firm, Figliozzli & Company, to perform the audits. According to CMS, prepayment audits will include random audits and “audits that target suspicious or anomalous data.” While the actual number of audits is unclear, Rob Anthony, deputy director of Health IT Initiatives Group for CMS was recently quoted as saying as many as 10% of program participants will face an audit.
Audit targets are contacted via email using the email submitted during the attestation process. The initial request asks for some basic information such name, NPI number, EHR Cert number, reporting period, the names of the offices or other outpatient facilities where patients are seen and whether CEHRT was deployed in those locations. The provider is asked to submit a copy of the “source document” which was used when the provider attested. In most case this will be a “dashboard” view of the MU measures and CQMs. Make sure this document includes the numerators and denominators for the measures reported, the time period the report covers (the reporting period) and evidence that the report was generated for the provider subject to the audit.
Supporting documentation
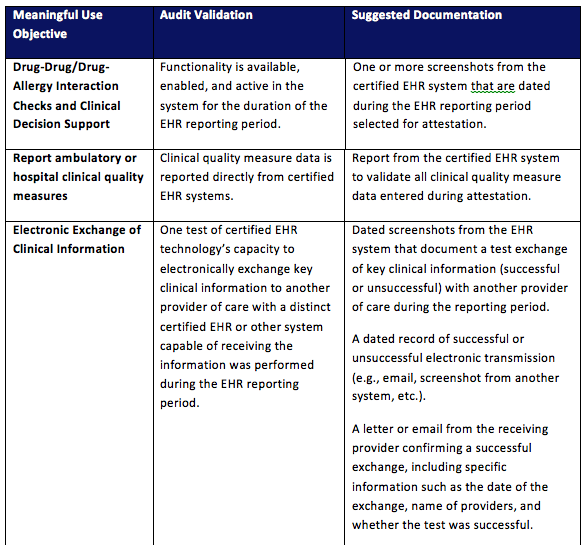
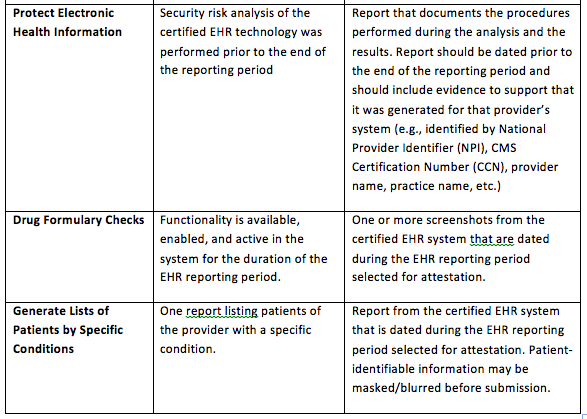
Finally, the audit will request supporting documentation for the measures that are not percentage-based. The CMS tip sheet for the audit process has suggestions for many of these measures. The table below is copied directly from this link.
The audit process is indeed necessary, but evil is a bit of a stretch. For those subject to an audit, there will be time invested in the process and perhaps a bit of anxiety waiting for a decision, which is delivered by way of an Audit Determination Letter. There is an appeals process for those who dispute the results of the audit, however if a provider is found not to be eligible for the incentive payment as a result of the audit, the incentive payment will be recouped.
Preparation
My advice to prepare for the possibility of an audit revolves around capturing and maintaining the required documentation. Remember, the audit process was clarified long after the EHR industry set about designing and certifying their applications. Take a close look at the non-percentage-based measures, and the measures for which you reported an exclusion. Look at the list in the table above and make sure you are collecting the appropriate documentation for your providers. CMS suggests retaining the documentation for six years post attestation.
Ten percent seems higher than what I am seeing in the nephrology space today. Of course, the audit process is not quite a year old and perhaps audits will become more common within our specialty as time passes. As the saying goes, an ounce of prevention is worth a pound of cure. Make sure your documentation is in hand, and hopefully you will never need to use it.



Leave a Reply