 March is well underway and workforce productivity is in the midst of a recurring springtime slump as that annual institution known as the NCAA basketball tournament is in full swing. If you were among the unfortunate few to pick the Spartans to win it all, you are in good company.
March is well underway and workforce productivity is in the midst of a recurring springtime slump as that annual institution known as the NCAA basketball tournament is in full swing. If you were among the unfortunate few to pick the Spartans to win it all, you are in good company.
Speaking of March, this month’s issue of Health Affairs includes a few articles that caught my attention. Although the articles about physician spend on quality programs, fee-for-service as the dominant payment method, and public reporting of surgeon-specific data were intriguing, it was the article about hospital EHR adoption that filled the gaps created by my busted bracket.
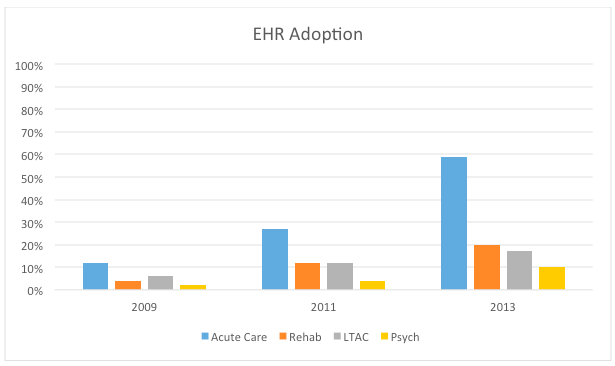
In their article entitled “Meaningful Use of EHRs Among Hospitals Ineligible For Incentives Lags Behind That of Other Hospitals, 2009-2013”1,Walker et al. highlight a remarkable disparity. Using data from an American Hospital Association survey, the authors compared the rate of EHR adoption between hospitals eligible for the meaningful use program and those that were not. The ineligible category included rehabilitation hospitals, long-term care hospitals (LTACs), and psychiatric hospitals. Not surprisingly, the facilities not in line for the MU dollars lagged behind those eligible to collect the incentive. What is surprising however, is the magnitude of the difference. I’ve reproduced some of the data in the bar chart below.
By the way, CMS reports that in 2015 over 95% of the acute care hospitals in the country were using a certified EHR. One might imagine the disparity Walker et al. have reviewed has substantially widened.
Dialysis & incentives
Even in a week of bracket-busting losses, one might ask why discuss this in a blog dedicated to the intersection of nephrology and health IT? Largely because dialysis facilities have something in common with LTACs, rehab facilities, and psych hospitals. Like the ineligible hospitals in the Walker study, dialysis facilities have been excluded from the meaningful use framework. And while adoption rates by dialysis facilities are not tracked, one might imagine they more closely resemble the ineligible hospitals than the acute care numbers.
This issue is important for another reason—unintended consequences. We’ve referenced one of my favorite books in this blog before. In Drive, Daniel Pink explores what motives individuals. If you don’t have time to read the book, spend 10 minutes watching this clever animation. But Pink’s discussion about autonomy, mastery, and purpose are not the topic today. No, what Pink and others have uncovered is the counterintuitive notion that if you try to motivate complex change by applying rudimentary “carrot and stick” incentives, not only are you unlikely to succeed, you may do worse than you would absent the inventive. And what could be more complex than adopting an EHR?
Unintended consequences
The real problem here is the creation of unintended consequences. There are several, but two come to mind in the midst of the Madness. First, because nephrologists take care of patients with ESRD, their encounters within a dialysis facility frequently outnumber their office-based encounters. Absent a certified EHR within the facility, thousands of nephrologists have filed for the MU hardship exception, effectively opting out of the MU program (and most whom I have spoken with are delighted this escape hatch exists). Second, in geographies where dialysis facilities have elected to deploy a certified EHR, they are compelled to charge nephrologists to use the EHR. Why? Because the financial benefit of using the EHR (i.e., avoiding the MU penalty) accrues to the nephrologist. Talk about an unintended consequence. Imagine if you had to pay every hospital for the privilege to use their EHR?
The winner is…
Much has been made of Andy Slavitt’s recent comments about the future of meaningful use. Coupled with the looming proposed rule for the implementation of MACRA, we may soon find ourselves in a new ball game. If that happens, understanding the rules of the game will be of paramount importance. Things are unlikely to change within the realm of LTACs, rehab facilities, psych hospitals, or dialysis facilities. But for nephrologists, the question on everyone’s mind is will the game get better or will it get worse? Unlike the Spartans, we will not have to wait until next season to find out.
Reference
1 Walker D, Mora A, Demosthenidy MM, Menachemi N, Diana ML. Meaningful Use of EHRs Among Hospitals Ineligible For Incentives Lags Behind That of Other Hospitals, 2009-2013. Health Aff (Millwood). 2016;35(3) 495-501.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.




Leave a Reply