Three days! That’s right, for those of you who share my tendency to procrastinate around this time of year, there are three days of shopping left—a virtual lifetime for the latent holiday shopper. And with the winter solstice behind us, think about all of the extra daylight we will see in the days ahead! As you scurry around looking for the perfect gift for that special Health IT nerd in the family, how about picking up a Learning Health System? Okay, I know what you’re thinking…Ketchersid is hitting the eggnog a little early this holiday season. But step out of the last-minute frenzy of the holiday season and let me explain.
JASON
The Learning Health System recently made the news when JASON, an independent group of scientists tasked with advising the U.S. Government on matters of science and technology, published a report entitled “Data for Individual Health.” Dugan introduced us to JASON a few months ago when she highlighted their report on data infrastructure. More recently, JASON was asked by the Agency for Healthcare Research and Quality (AHRQ) to answer a simple question:
How do we move from a system focused of the care of individuals to one focused on the health of individuals?
Piece of cake, right? AHRQ kindly framed the question by specifically asking:
- How can EHRs highlight opportunities to engage individuals as they try to achieve health, and to learn from failed efforts to improve treatments for individuals?
- How would an EHR of the future help a care team whose goal was health, rather than health care, and who, along with the individual, have access to all the data?
- How can data analytics be used to support high quality, patient centered care and offload the large requirements of processing?
Learning Health System
Tough to summarize an 80-plus-page report in 800 words, and I know you have a few more gifts to pick up today, but suffice it to say one of the underpinnings of the solution proposed by JASON is a closed-loop Learning Health System. According to JASON, the delivery of care today is hampered by the open loop depicted in figure 2-1, which I borrowed from the report:
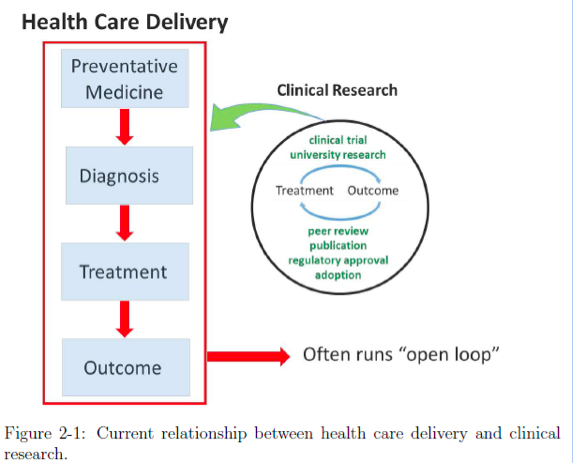
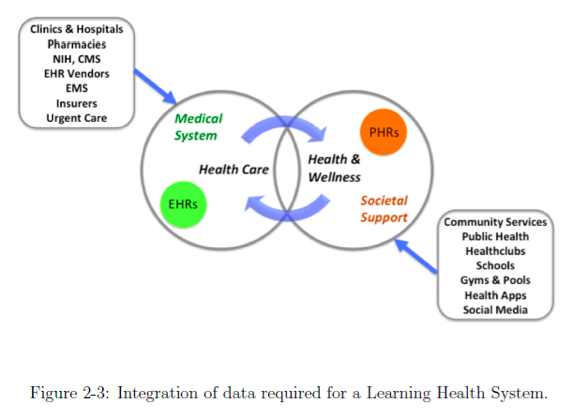
The problem in JASON’s eyes is that real-world outcomes data do not inform the health of the individual. The framework for the solution is to close the loop as depicted in figure 2-3 from the report:
Recommendations
So, how do we get from the first figure to the second? Let’s just say it’s a remarkably heavy lift, but JASON has a few suggestions, most of which are directed at Health and Human Services (HHS), which seems appropriate as they asked for the study in the first place. Again, liberally copying and pasting from the report, JASON leaves us with eight recommendations including leveraging the data infrastructure piece Dugan shared with us in August:
- It is time to act on the broad agreement found in past reports regarding health information. HHS should take the lead in harmonizing the recommendations and promoting paths forward. HHS should establish a framework for measuring progress along these paths.
- HHS should adopt standards and incentives to allow sharing of health data. HHS policies should require that metadata and provenance be associated with all data so that data quality and use can be evaluated.
- HHS should adopt policies of support for proposed open API standards. These policies should make it advantageous for one or more leading EHR vendors to be the first to propose such standards. HHS should recognize ecosystem-friendly EHRs as a public good. HHS should adopt reimbursement differentials, initially small, for institutions that adopt ecosystem-friendly EHRs.
- HHS, in partnership with private foundations, should establish “race to the top” challenges for community involvement. These would seek to demonstrate, through the integration of community services and broader wellness services, a measurable increase in health and wellness, and a concomitant reduction in the number of encounters with the health care system.
- Relevant non-profits should be encouraged to assess their goals with respect to health data streams, and to provide “stamps of approval” for applications (apps) and other consumer tools. This will speed adoption of these tools.
- Accrediting bodies should require training of all health care team members to achieve required levels of numeracy and fluency in a common parlance of health informatics. Professional schools should develop continuing education and certification programs that cross-educate team members regarding the diverse informatics expertise required by the team.
- FDA and other agencies should seek a nuanced approach to adjudicating the regulatory line. Products and services that now risk being construed as “practicing medicine” could be allowed to exist in a more nimble regulatory space that fosters rapid innovation and adaptation to new developments while mitigating concerns over demonstrated accuracy. For example, products and services in this space could be subject to a requirement to simultaneously report information to the designated health care team, as well as to the consumer, as a risk mitigation strategy.
- HHS should accelerate the development and adoption of a robust health data infrastructure based on the principles outlined in the ONC 10-Year Vision and other consensus studies.
Stocking Stuffer?
If you are still reading this post you certainly recognize this is quite a bit more than a stocking stuffer, but the implications for health IT and nephrology are worth considering. Over a quarter-of-a-million physicians will face the 1% penalty in 2015 for failing to demonstrate meaningful use. That figure will likely rise in 2016 as more providers jump ship rather than weather the Stage 2 storm. Next summer HHS will publish the proposal for the next round of the meaningful use program. Increasingly we are hearing calls for interoperability, and an open API requirement, for example, is not outside the realm of possibilities. As health care providers, it can be difficult to look beyond the delivery of care to our patients. But the notion of shifting the focus from the care of the individual to the health of the individual has wide appeal. Perhaps we will see this one under the tree in the years ahead. In the meantime, all of us at the Acumen blog would like to wish you and yours a safe and happy holiday.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.




Leave a Reply