
Well Acumen blog faithful, it’s hard to believe the end of October is just a few days away. With little fanfare, but in the face of substantial anticipation, the request for application (RFA) for CMMI’s new voluntary models was released late last week. Pure coincidence that its release was one week before Halloween? I’ll let you be the judge of that! As previously noted, there are four new voluntary models, now collectively known as Kidney Care Choices (KCC) models…gotta love all the new acronyms! Today, let’s walk through what we’ve learned from the RFA about the “simplest” of the four, Kidney Care First (KCF).
RFA
First, let’s make one thing clear. While the RFA sheds a lot of light on what we can expect from the new models, there is still a truck load of detail missing. Most of it is missing because CMMI is working out some of the details, which means they still may be open to suggestions. At a high level, the way this works is interested nephrology practices will submit an application to CMMI before January 22, 2020. CMMI will review and accept the applications of those found worthy. Accepted applicants will receive an Implementation Period Participation Agreement to sign. This stands up the KCF entity for 2020, when there is no financial risk. Sometime between signing that agreement and the end of 2020, the KCF will sign a Performance Period Participation Agreement. This last agreement will contain all of the detail you need, which is a good thing because when you sign that one, you are all in, and fully exposed to the ups and downs described below.
Size matters
First a few basics. A KCF is formed by one or more nephrology practices. No other providers can actively participate in KCF. Once it is formed, CMMI aligns patients to the KCF based on encounters the nephrologists in the KCF have with adult Medicare beneficiaries. The KCF will have a CKD population that consists of stage 4 & 5 patients and an ESRD population. There is a ton of detail regarding who is eligible and how alignment works, but at the end of the day, if you provide the MCP service for an eligible dialysis patient, they are in your KCF. If you have at least 2 E&M visits in 6 months with a stage 4 or 5 patient, they are in your KCF. So why does size matter? KCF has a minimum patient count. To stand up a KCF you need to have at least 500 late stage CKD patients and at least 200 ESRD patients.
Sounds easy right? Well, when you look at the eligibility criteria, I think this may require practices with at least 5 to 7 docs to be on the safe side, but that’s just a guess. And when the 21st Century Cures Act comes to fruition in 2021, the number of primary Medicare patients we see on dialysis will decline. Not the end of the world, but if you like this model and you are a small- to medium-sized practice, you may want to start looking for a partner.
Show me the money
Okay, not to be crass, but this is a new payment model…how are we getting paid? Well, if your practice lands in KCF, starting in 2021, there are three revenue streams, each, of course, with its own acronym:
- Kidney Transplant Bonus (KTB) – easily one of the most attractive features of the KCC suite of models
- Adjusted Monthly Capitation Payment (AMCP)
- CKD Quarterly Capitation Payment (CKD QCP) – my least favorite new acronym
Let’s take each in turn and unpack them based on what we see in the RFA.
Kidney Transplant Bonus
Let’s start with the good news. Truly the sweetest treat in this complex morass! Let’s assume our practice signs up for KCF. We have a panel of aligned stage 4 & 5 CKD and ESRD patients. Now one of them receives a renal transplant (deceased donor, living related, kidney pancreas…the source does not matter). Fast forward a year. Is the transplant still functioning? If so, CMS writes us a check for $2,500. Two years out, kidney still functioning, patient has not returned to dialysis? They write another check for $5,000. Finally, three years out and the transplant is still functioning, we receive a third check, this one for $7,500. That’s $15,000 over three years if the transplant is still working! Best I can tell, there are no hidden “gotchas” here. CMMI recognizes this is the best way to treat ESRD, and with a bonus like this, every one of us will become even greater advocates for transplant than we are today, if that’s possible.
Adjusted MCP
Here’s where things become interesting. KCF will make prospective payments to basically cover the outpatient care for the aligned patients. For the ESRD patients, that payment is referred to as the “Adjusted” MCP. This is a single payment to cover what the MCP covers today. You will still submit CPT codes for the MCP to CMS, but those codes will not be paid individually in KCF as the service is now covered by the prospective payment. The interesting part is the rate they intend to pay in these models is the 2-3 visit-in-center rate. Let me repeat that, out of the gate, your base payment for every ESRD patient in the model is pegged at the 2-3 visit-in-center rate. So regardless of whether you see a home patient and regardless of how frequently you see an in-center patient, you are paid the same. I’ll let you do the math, but while the 2-3 visit-in-center CPT code is reimbursed at about the same rate the home MCP CPT code is, the reimbursement is around 75% of the 4+ visit-in-center CPT code. In case this sends you into a tailspin, grab a cup of coffee and keep reading as this prospective payment along with the CKD prospective payment will be adjusted up or down based on performance. More on that later.
CKD QCP
This one is also worth your undivided attention. Basically, CMMI will bundle a series of outpatient CPT codes and make one prospective payment every quarter to cover those services. The codes included in the CKD bundle are displayed in the table below.
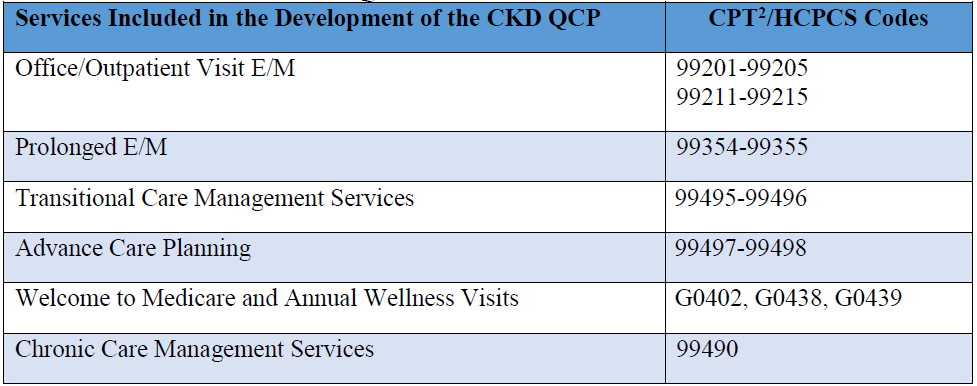
In some fashion this prospective payment works like the MCP we’ve been used to. You will still submit the CPT codes when one these encounters occurs, but CMS will make a payment each quarter to cover all of the services listed above. If you deliver a service not on this list to an aligned CKD patient, you will be paid by Medicare as you are today. CMMI has decided to establish the base rate for this bundle such that it is equivalent to 1/3 of the MCP payment noted above (the 2-3 visit-in-center rate). They also intend to adjust this payment for “leakage”. Not that it would happen to an Acumen blog reader, but suppose an aligned CKD patient decided your care was substandard and they elected to receive services in the CKD bundle elsewhere. If that happens, CMMI intends to reduce your prospective payment. And like the Adjusted MCP, the CKD QCP will be adjusted based on performance as described below.
Quality gate
Within KCF we will receive two prospective, population-based payments, one monthly (MCP) and one quarterly (CKD). Before we discuss how those payments will be adjusted, let’s explore how we will be measured. The first order of business is the quality gate. CMMI will determine how our KCF does with respect to three quality measures:
- Gains in Patient Activation Scores at 12 Months (NQF #2483)
- Depression Remission at 12 Months – Progress Towards Remission (NQF #1885)
- Controlling High Blood Pressure (NQG #0018)
We can quibble about the selected quality measures, but you also need to consider, how will you get the quality data to CMMI? While it’s not mentioned in the RFA, I suspect they will lean on the methods employed today through MIPS. But let’s not underestimate the operational overhead necessary to collect the data for these “intriguing” quality measures.
Utilization measures
In addition to a quality gate, our performance will be measured against the three utilization measures listed below:
- Optimal ESRD Starts (NQF #2594)
- Hospitalization Costs (a mash up of the NQF Standardized Hospitalization Ratio)
- Total per Capita Costs (an existing cost metric within MIPS)
As with the quality gate, the performance of our aligned stage 4 & 5 and our aligned ESRD patients will be regularly measured by these three utilization measures. What does CMMI intend to do with the quality gate and these utilization measures?
Performance-based adjustment
If you are still reading this lengthy post, this part is probably worth waiting for. Let’s assume our KCF has 500 ESRD patients and 1,000 CKD patients. At the beginning of each month, CMS will pay the KCF 500 times the prevailing rate for the 2-3 visit-in-center MCP, and at the beginning of each quarter, they will pay the KCF 1,000 times the prevailing rate for the 2-3 visit-in-center MCP (recall the CKD payment is equal to 1/3 of the 2-3 visit-in-center MCP, so effectively we are paid the equivalent of the 2-3 visit code to treat a CKD patient for three months). But remember, KCF is intended to be an Advanced APM starting in 2021, and one of the critical components of an Advanced APM is financial risk. KCF meets that requirement through the performance-based adjustment (PBA—yes, another acronym). The PBA has some complexity to it, but bear with me and we will get through it!
The PBA is basically an assessment of the KCF’s performance against the utilization measures, with a quality gate speed bump up front. We will be measured initially against our peers (the so-called relative performance component of PBA), and then later they will add an improvement piece (referred to as the continuous improvement component). When both achievement and improvement are in play, the top end of this adjustment will be a 30% bonus added to the MCP and CKD payment, and the bottom end will be a 20% penalty. Reading between the lines, in my view, it will be extremely rare for a KCF to capture the 30% bonus, and likewise, your KCF would have to be terrible (or very unlucky) to face the 20% haircut. But let’s walk through the thing and let you decide for yourself.
Relative performance
Think of the PBA calculation as sequentially stepping through three questions:
- Did we clear the quality gate?
- If so, how did we perform on the utilization measures vs our peers in other KCFs?
- If we are in the bottom half of the class with respect to our KCF peers, how did we perform compared with the nation’s nephrologists?
Those questions will be answered every six months and those answers will put us in one of eight levels. These eight levels basically determine what adjustment CMMI will apply to our prospective payments for a six-month period. If we don’t clear the quality gate, we are assigned to level 8 (you really don’t want to be in level 8). If we clear the quality gate, and we are in the top half of our class of KCF peers, pat yourself on the back and take the check to the bank! Top 10% lands in level 1, next 10% level 2, and so on down to level 5. Levels 1-5 are guaranteed to see a bump in their prospective payments during this six-month period.
As for those in the bottom half of the class, you get to face the third and final question. Are you in the bottom half compared with your KCF peers, but the top half of the nation with respect to the utilization measures? If so, welcome to level 6. Find yourself in the 25th to 50Th percentile nationally, you are in level 7. If you unfortunately are in the bottom quartile of the nation, you face the dreaded level 8. For the visual learners in the audience, check out the table below.
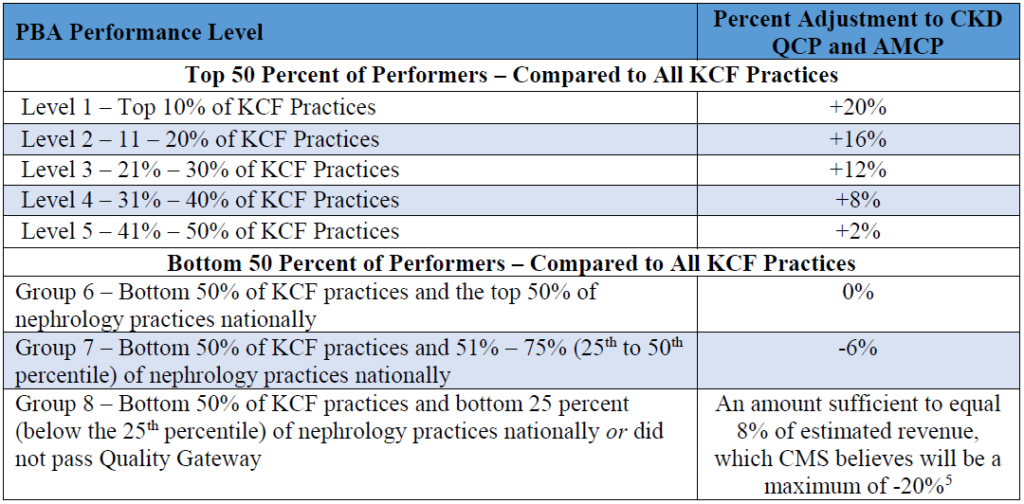
To be clear (because this is very confusing), during the first half of 2021, my KCF will be measured. Those results will be tabulated in the second half of 2021. If, during the first half of 2021, I clear the quality gate, and compared with my KCF peers my performance across the three utilization measures is in the top 21 to 30% of every KCF during the first half of 2021, then in the first half of 2022, each adjusted MCP and CKD quarterly capitation payment I receive during those 6 months will be 12% higher than the base payment. Clear as mud, right? But wait, there’s more!
Continuous improvement
Later in the program, as I establish a baseline of sorts, my KCF will also be eligible for an improvement bump to the PBA. Starting in performance year 2 (2022), if my KCF clears the quality gate, we are eligible for the improvement bump. Now this gets a little tricky. CMMI intends to look at my KCF’s performance on the three utilization measures during the first half of 2022, and compare that with our performance during a prior six-month period. The amount I must improve and the reward I receive for hitting that target vary based on which level I find myself in (in case it’s not apparent by now, your level is very important!). The table below describes both the improvement targets and the reward for hitting the target for each level.
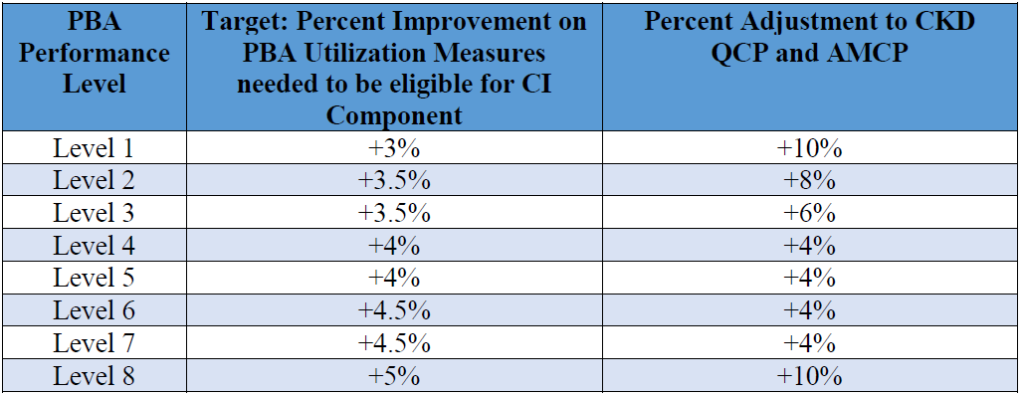
Once again, to be clear, if my KCF is in level 3, and my performance on the three utilization measures improves more than 3.5% compared to where we were in a prior period, I get an additional 6% added to my Adjusted MCP and my CKD QCP for the next six months. I don’t know about you, but my head is swimming. 😉
All together now
At the end of the day, you are being paid a prospective payment to cover the outpatient services you deliver to the late-stage CKD and ESRD patients aligned with your KCF. The MCP payment is discounted to the 2-3 visit-in-center code out of the gate. The CKD bundle payment is either higher than what you receive today (if you rarely see your CKD patients) or it is discounted (if you see those patients a lot today). In KCF, you are putting those outpatient professional fees at risk in this model. As the model moves down the path, those base payments are adjusted up or down based on your performance against three utilization measures (I am assuming not a single Acumen blog reader will fall below the quality gate—don’t let me down!). The table below is an attempt to tie together both the relative performance and continuous improvement components of the PBA.
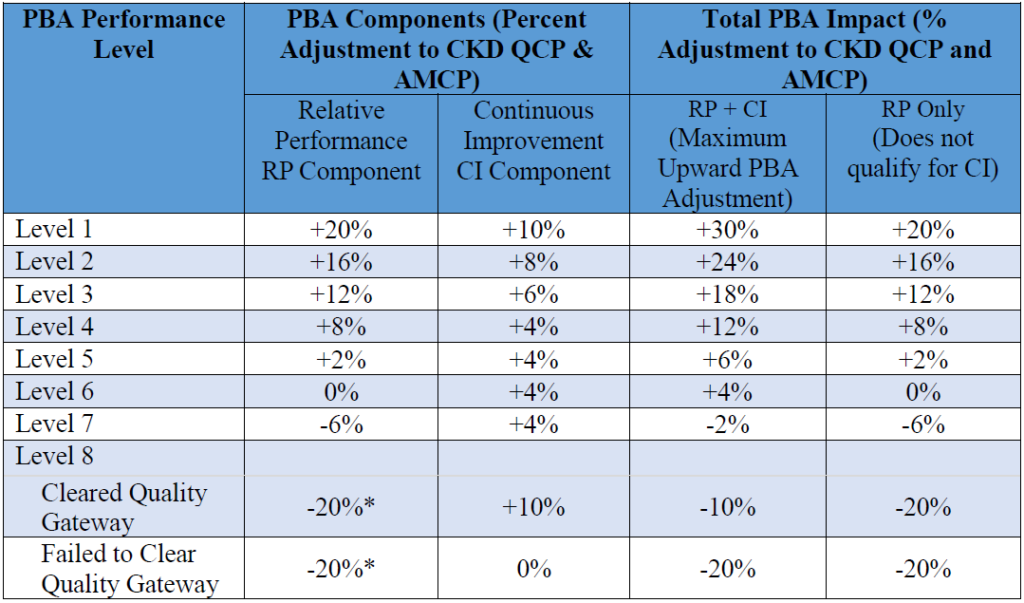
The column far right is PY1 prior to the availability of the improvement piece, and the column to its left with the big numbers represents the maximum upside one will see applied to the prospective payments starting in performance year 2.
Trick or treat?
At first blush, this thing is massively complex. As I type, this beast is just over 72 hours old, and I’m still wrapping my head around it. As you consider the pros and cons, let’s not forget KCF is intended to be an Advanced APM, and when the ESCOs ride off into the sunset at the end of next year, there remain two more years where qualifying participants in an Advanced APM are handsomely rewarded. Of course, the decision to apply is up to each practice. Is your practice large enough to go it alone? What’s your appetite for risk? Who will your KCF peers be? What’s the cut point for the quality gate? And, of course, countless other questions not answered by the RFA.
While you noodle on those questions, the Acumen blog team hopes that you and yours have a fantastic and safe Halloween. Oh, and those CKCC models? I suspect you will hear about those in a future post. Trick or Treat!

Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Image from www.canstockphoto.com




Jeremy Yospin says
Does this model expect nephrologists to be the PCP for all CKD 4-5 patients? Will the “leakage” apply to other specialist visits (i.e. cardiology, GI) who will also submit 9920x and 9921x codes?
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Great questions Jeremy. My read is they do not intend for the nephrologist to become the primary care provider, but they are leaning towards asking the nephrologist to become the “principal” care provider. With regards to leakage, I think they will establish a base rate (denominator would be all encounters in the CKD bundle with any provider, numerator would be same bundled services, but provided by the nephrologist). Over time, if that fraction becomes smaller, they will assume aligned patients are seeking services elsewhere, and if that happens they will adjust the cap payment down a bit.
Jung Hoon Son says
“so effectively we are paid the equivalent of the 2-3 visit code to treat a CKD patient for three months”
Might be misunderstanding but – shouldn’t it be “four months” since its 1/3 of 12 months?
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Apologies for the confusion Jung. The base rate they intend to pay is the 2-3 visit in center rate per ESRD patient per month. They will pay the same rate to care for a CKD patient for 3 months. On a month by month basis, the CKD payment is 1/3 of the ESRD payment.
Jung Hoon Son says
Thank you for the clarification. Once I tried to calculate sample numbers I was forced to calculate monthly ESRD MCP in order to get the CKD QCP, so now makes much more sense.
Also, this is a fantastic summary of the KCF model. Thank you!
-Jung
Chris Najafi, MD says
If you sign both agreements, it there an out anywhere down the line?
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Yes Chris there is. Basically this works as follows; submit an application (for KCF, CKCC or both). CMMI reviews the applications and decides who to accept. Then you get an Implementation Period Participation Agreement to review and sign. This puts you in play during CY 2020 when there is no downside risk. Finally, between then and the end of the year you will see a Performance Period Participation Agreement. Signing this one locks you in to 2 years. You can get out, but it will cost you.