
Welcome to the new decade, Acumen blog readers. Have you gotten used to typing or writing 2020? Neither have I! As we break new ground this decade, one of the things on our minds is the new nephrology payment models announced by CMMI last year. We’ve heard absolutely nothing about the proposed mandatory ESRD Treatment Choices model, so our attention today turns to Kidney Care Choices. Kidney Care Choices (KCC) is the moniker for the 4 new voluntary models. The application deadline for these models has come and gone, but one thing that remains top of mind for many nephrologists is this: How will these new payment models impact my bottom line? While the short answer is “it depends,” let’s devote today’s post to making this murky pond a little clearer. Apologies in advance for the length of this post, but this stuff is complicated!
Let me start by pointing out I am not the first one to dip my toe into this morass. The ASN recently made a run at this by publishing a payment calculator which compares today’s fee for service (FFS) payments with what one might expect to see in Kidney Care First. I applaud the effort by ASN, but I think most nephrologists using the calculator may elect to use the default entries, which could lead to some challenges due to the nuance of this complex problem. What follows is a different perspective, informed by my understanding of the new payment models and access to data sets that provide additional insight (many thanks to Dan DeFalco and Nephrologixx). As a quick reminder, yours truly no longer practices nephrology and heaven forbid if I were to provide you with financial advice, so take this post with a grain of salt. 😉
Getting started
One way to think about the financial impact nephrologists will face in these models is to divide this topic into two buckets:
- Direct impact on monthly cash flow, and
- Everything else
There are two items that impact monthly cash flow, the Adjusted Monthly Capitation Payment (AMCP) and the CKD Quarterly Capitation Payment (CKD cap). Although likely stating the obvious, recall the only patients impacted are the aligned Medicare primary ESRD and CKD stage 4 and 5 patients, and the model only applies to 80% of the Medicare allowable for the services under discussion.
AMCP
As previously noted, all ESRD patients aligned to these models will be paid at the 2-3 visit in-center HD rate. As I know all of you are aware, the 2-3 visit in-center HD rate is nearly identical to the home dialysis MCP payment. Why is this important? If you look at what’s called the Medicare 5% sample, as noted in the ASN calculator, the difference between the average fee-for-service (FFS) payment for the MCP today and the anticipated AMCP payment in the KCC models is about $30 per patient per month (PPPM). If you use the default on the ASN calculator, the answer is that your practice will earn $30 PPPM less in KCC for every aligned ESRD patient. That’s true if you are the “average” nephrologist. But as my favorite actuary likes to remind me, no one is average. The “average” nephrologist has an average home dialysis rate. And when it comes to the frequency with which he/she sees in-center hemodialysis patients, the rate at which he/she manages to make 4 visits each month is also “average”. But consider the following:
- If you have a high home dialysis rate and your 4 visit in-center dialysis rate is low, the impact of the AMCP will be less than the $30 PPPM haircut mentioned above.
- On the other hand, if your home dialysis rate is low and you have a high 4 visit in-center dialysis rate, the impact of the AMCP will be greater than the $30 PPPM haircut—perhaps much higher.
CKD cap
Now for the tricky piece of this puzzle. As previously noted, stage 4 and 5 patients are aligned to these 4 models when the patient has at least 2 of the encounters in the table below with a nephrologist, within a 6-month time span.
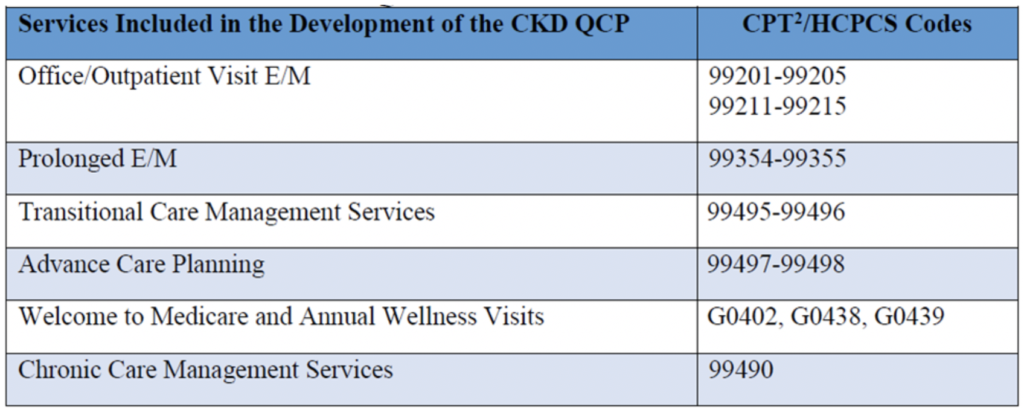
The CKD cap is an upfront quarterly payment that’s intended to cover every service in the table, delivered to an aligned stage 4 or 5 patient during the 3 months in the quarter.
The ASN calculator allows a practice to enter its CKD E&M claims, but very few practices actually know this number, or understand what they should include in the number. The answer is 80% of the allowable for the codes in the table above that they deliver to Medicare primary CKD patients who qualify for alignment. That number is remarkably difficult to tease out of a typical nephrology practice revenue cycle platform. So how should we deal with that? Well, we could start with a “least common denominator” approach of sorts. Suppose the way my stage 4 and 5 CKD patients are aligned to my model is that, like clockwork, I see them every 3 months and bill an outpatient E&M visit. Cast your eyes on the table below:
| CPT code | 80% of Allowable | CKD Cap Benefit (PPPM) |
| 99213 | $60 | $42 |
| 99214 | $86 | $33 |
| 99215 | $116 | $23 |
A few important caveats here. Your Medicare payments will obviously vary based on geography, but for the sake of argument assume these are directionally correct. The CKD cap pays the 2-3 visit in-center rate on a quarterly basis, or roughly $185 per patient per quarter. Minimum alignment criteria would mean delivering one of these CPT codes every quarter. For example, for 99213, the CKD cap pays $185 vs the $60 you collect today in FFS, meaning you collected an extra $125 per quarter or $42 PPPM as noted in the third column. Clear as mud, no?
At first glance, this looks like a wonderful gift. It looks for all the world like we are being paid very well to care for late-stage CKD patients. But are we? And if we are, is it enough to overcome the AMCP haircut?
Alignment and payer mix
As nephrologists, we all know we see more CKD patients than ESRD patients, right? But a funny thing happens when you zoom in on a single payer like Medicare. If you compare the payer mix in your practice for patients with ESRD and for patients with stage 4 and 5 CKD, you will likely see that a higher percentage of your ESRD patients are covered by Medicare when compared with the percentage of late-stage CKD patients covered by Medicare. This is largely related to the way the Medicare ESRD benefit works. Couple this payer mix mismatch with the necessity to see CKD patients twice in 6 months in this model and the CKD:ESRD ratio is inverted. When we look at internal data sets and include the alignment scheme used in KCC, the CKD:ESRD ratio across nephrology practices is as low as 0.3 and as high as 0.7 for these models. This is important because most practices rely on monthly cash flow to pay the bills. And if you are taking a haircut on the AMCP, you must overcome that monthly cash flow hit with the CKD cap. I am here to tell you that’s a very tall hill to climb unless this model changes.
All together now
So, what does this all mean? First, I hope I have convinced you there is no such thing as an “average nephrologist.” But assume for the moment we could get comfortable with the math that says the AMCP is going to cost us $30 PPPM vs what we collect today in Medicare FFS. What would it take to overcome that cash flow hit? Well, if the only thing we do for late stage CKD patients is see them in the office every 3 months, and the only code we use is 99213, and we are on the very high end of the inverted CKD:ESRD ratio, we might break even. But let’s face it, most of us will have substantially fewer CKD patients than ESRD patients in this model. And many practices have let me know they appropriately use 99214 or 99215 for these complex patients and they are delivering CCM and TCM services for their stage 4 and 5 patients. Again, looking at internal data sets, the net impact of AMCP and the CKD Cap payment appears to be a monthly cash flow hit that ultimately amounts to between $4,000 to $10,000 per doctor per year. And that’s not including the mysterious impact “leakage” could have on the CKD cap. Thankfully, this is not the end of the story.
PBA
I do not intend to revisit the impact the performance-based assessment (PBA) has on the AMCP and CKD cap payment in Kidney Care First, but the PBA is an important consideration for those of you considering KCF. You can review the complexity involved with the PBA here. Suffice it to say, those in KCF will be paid in the same fashion as those within CKCC during the first year of the model. After that, the AMCP and CKD cap are adjusted up or down based on how the practice performs compared with other model participants. The ASN calculator highlights the impact each PBA level will have on your payments. But it’s important to recognize that every practice in KCF is competing against every other practice in KCF. Stated another way, in the later years of KCF, there will be winners who see increases in the base payment rates, and there will be losers who face even more dramatic monthly cash-flow impairment than those described above.
Everything else
Beyond the impact the AMCP and CKD cap payments will have on monthly cash flow, nephrology practices are also considering the impact of as many as 3 other sources of revenue in these new models:
- The transplant bonus
- The Quality Payment Program (QPP) impact of participating in an Advanced APM
- The potential to share in total cost of care savings within CKCC
Transplant bonus
As noted in a prior post, the transplant bonus is perhaps the most attractive feature of KCC. It is paid based on the anniversary dates of successful transplants. Assuming the transplant is functioning on the anniversary date, the payments are $2,500 in year 1, $5,000 in year 2 and $7,500 in year 3. From an operational perspective, CMMI intends to make these payments quarterly, such that if an aligned patient has a functioning transplant 1 year out, your $2,500 check should be received within 3 months of that 1-year anniversary. It’s my understanding that in a typical year roughly 9,500 Medicare beneficiaries receive a kidney transplant. That’s remarkably similar to the number of nephrologists in this country. So, assume for a moment that among the Medicare patients aligned within these models, one of those aligned patients receives a transplant per nephrologist per year. (I know there’s no such thing as an average nephrologist, but bear with me.)
Let’s also assume the 3-year organ survival rate is 100%. With this in mind, sometime in performance year (PY) 2 a doc in the model will receive $2,500 because the lone aligned Medicare beneficiary that received a kidney in PY 1 had their first anniversary. Rolling forward one year, sometime in PY 3 the practice would receive $7,500 ($5,000 for the year-2 anniversary for the first patient and $2,500 for the year-1 anniversary for the kidney transplant that occurred in in PY2). Using the same logic, the following year it’s $15,000, as it would be for subsequent years. Bottom line, this is fantastic incentive, but from a cash flow perspective you will wait for this one. But if you are willing to wait, it looks like the transplant bonus will rescue your cash flow worries during the last few years of the model.
QPP
And speaking of waiting, those of you in the ESCO program know all about waiting for the 5% payment you receive as a Qualifying Participant in an Advanced APM. This bonus is applied to what amounts to your entire Part B book of business and can be a sizeable sum (similar in magnitude to the later years of the transplant bonus). But again, you will wait for this. 2021 is PY 1 for KCC. If you are a Qualifying Participant in one of these models in 2021, the Advanced APM bonus will likely be paid in the second half of 2023. And recall, 2021 and 2022 are the last performance years for this bonus. The alternative to the Advanced APM path is exposure to the Merit-based Incentive Payment System, affectionately known as MIPS.
CKCC
Last but certainly not least, those of you who sign up for CKCC will also be in line to share in savings achieved for reducing the total cost of care in these models. Of course, if things go sideways, you are also liable for some of the losses incurred (just like in the ESCO program). It’s far too early to guesstimate what the impact will be for this aspect of the program. But for the sake of full transparency, it does deserve mention because there is a decent chance this is where the real opportunity lies for nephrologists willing to take risk. But again, you will not feel the financial benefit that’s recognized by reducing the total cost of care until late in the KCC game.
The calculator
Where does this leave us? Well, back to the ASN calculator. I think this is a good start, but be careful if you elect to use the defaults. None of your practices are “average” and you truly need to understand the levers in these payment structures. From an immediate cash-flow standpoint, think carefully about:
- Your home dialysis rate
- The 4 visit rate for your in-center HD patients today
- The intensity of service you deliver to late-stage CKD patients today
- And remember, although it’s counter intuitive, the alignment scheme and payer mix almost guarantee that you will have fewer CKD patients than ESRD patients aligned in these models
Today’s conversation has been all about the potential impact you may face from a revenue perspective. Monthly cash flow keeps the lights on for many practices, and of course there will be some administrative expense coming out of that cash flow to capture and report on the new quality measures. I think CMMI has made some improvements in KCC when compared to the ESCO, but they missed the mark in my view with respect to payments to nephrologists. Professional fees collected by nephrologists represent a trivial slice of the total cost of care for this patient population. Discounting the payment to the nephrologist in these models makes little sense to me. Long story short, in my view CMMI has work to do on the cash flow piece of this puzzle, particularly in the early years of the model.
What are your thoughts about the payment structure within KCC? Let your voice be heard! Drop us a note and join the conversation.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Photo by Michael Longmire on Unsplash




Jeremy Yospin says
Some issues I wasn’t able to see answered in the RFA that may also affect the calculation:
1. How is “2 visits in 6 months” defined – the number of patients would be different if the six months starts with the first claim vs a fixed time period.
2. How is this program funded? This may be an issue for the transplant bonus – 50% of the bonus is paid 3 years AFTER transplant. So a patient who is transplanted 6 months into year 1 will reach this point in mid year 4. The program may not even exist then (year 4 and 5 I believe are optional add-on years). Will doctors still get paid the $7500 after the program ceases to exist?
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Great questions Jeremy. Regarding the first question, it appears that when the risk potion of this officially begins 1/1/2021, CMMI will look back over the preceding 6 months to determine which CKD patients to align. Then moving forward they will update the alignment in a prospective fashion. Regarding question 2, the expectation is that yes the payment for the transplant bonus will continue for the entire 3 years. I hope to see that confirmed when we have the participation agreements in our hands. Much of the missing detail should be in the PA.