Imagine seeing patients in the year 2024. You are in clinic and the first patient is a 63 year old male, referred by a local primary care physician for proteinuria. He was in the hospital two weeks ago and had a “bunch of tests” done. He arrives with no records. You fire up your trusty mobile device, speak a few words and, voila, in moments the pertinent pieces of medical history are at your fingertips. Science fiction? Perhaps, but the 10-Year Vision Statement recently released by the Office of the National Coordinator hopes to bring us closer to this information-sharing nirvana.
We’ve discussed interoperability in this blog before, but today I’d like to liberally quote from the above referenced report as I believe it provides a window into the direction HHS is moving. The report establishes 3-year, 6-year, and 10-year targets. The use-case examples provide a glimpse into what we are likely to see in the near, and perhaps long term. Categorized by target year those use cases include:
2017
- Individuals look up their electronic immunization histories as needed.
- Primary care providers share a basic set of patient information with specialists during referrals; specialists “close the information loop” by sending updated basic information back to the primary care provider.
- Hospitals automatically send an electronic notification and care summary to primary care providers when their patients are discharged.
2020
- Individuals regularly contribute information to their electronic health records for use by members of their care team.
- Individuals integrate data form their health records into apps and tools that enable them to better set and meet their own health goals.
- Primary care providers and authorized researchers are able to understand how well controlled the glucose levels (i.e., A1C values) of diabetic patient populations are and how often those patients have been hospitalized based on standardized information from multiple sources.
- Clinical settings and public health are connected through bi-directional interfaces that enable seamless reporting to public health departments and seamless feedback and decision support from public health to clinical providers.
2024
- Individuals manage information from their own electronic devices and share that information seamlessly across multiple electronic platforms as appropriate (health care providers, social service providers, consumer-facing apps and tools, etc.).
- Primary care providers can select effective medications for patients with certain conditions based on their genetic profiles and results of comparative effectiveness research.
- Individuals, care providers, public health providers, and researchers contribute information and learn from information shared across the health IT ecosystem, with rapid advancement in methods for deriving meaning from data without sharing PHI.
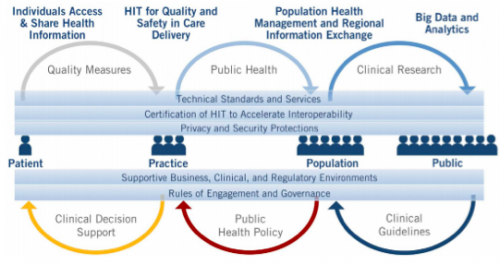
Sound ambitious? Perhaps, but from reading the 10-Year Vision Statement it certainly sounds like HHS intends to use the tools available to them to shift the focus from EHR adoption towards interoperability. At a high level the intent is to develop an agenda that focuses on five building blocks, again liberally quoting from the report:
- Core technical standards and functions
- Certification to support adoption and optimization of health IT products and services
- Privacy and security protections for health information
- Supportive business, clinical, cultural, and regulatory environments
- Rules of engagement and governance
Summary
What insights exist in this 10-year vision? I think there may be several. First, the example use cases mentioned for 2017 are on some of the lists I have seen regarding the Stage 3 meaningful use objectives. Remember 2017 is now the first year any provider will face Stage 3. Second, there is a very clear focus on facilitating the patient’s participation in their health care by providing access to and interaction with their electronic health information. “Patient engagement” has received a lot of interest lately; the vision outlined by ONC certainly supports this aspect of health information technology. The last insight is the fact that primary care providers remain central to the care team from the perspective of ONC. They are viewed as the captain of the ship. As nephrologists, we frequently fill this role for the ESRD population and we need to make sure national policy makers understand this.
The image below is a graphical representation from the report of the health IT ecosystem.
Achieving interoperability across this ecosystem is a necessary step to ensure the right data is available to the right people at the right time. Ten years sounds like a long time, but of course there is a tremendous amount of work to be done. Do you think we will get there? Let us know what you think by participating in our survey, and if I show up in your waiting room with proteinuria 10 years from now, I will make sure I bring my records.
[poll=”3″]




Leave a Reply