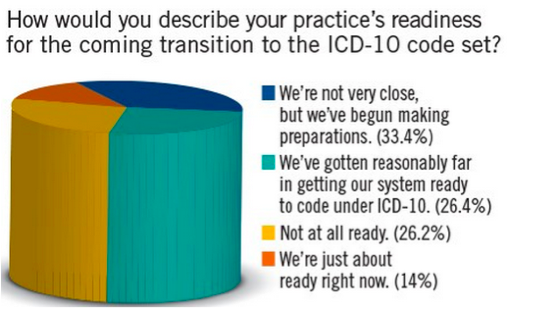
51 days to go. That’s right, we are indeed in the home stretch. In less than eight weeks the ICD-10 transition will be upon us. In spite of the looming deadline, many practices are not ready. Check out the graphic below from a recent technology survey conducted by Physician Practice. Granted the target of this survey was a general medical audience, but the results do not inspire confidence regarding ICD-10 readiness!
Last month Diana provided us with welcome news regarding the establishment of a 12-month grace period. As Diana pointed out, during the grace period CMS plans to pay for claims that are accompanied by an ICD-10 code that’s not as “specific” as it could be. While this is indeed welcome news, more recently CMS has clarified the details with a posted FAQ, which they seem to update on a weekly basis. As with all things from the agency, the devil is in the detail.
Looking under the covers
Let me start with the disclaimer that I am the last guy who should be providing billing and coding advice, but a few things are clear. First and foremost, the grace period only applies to claims submitted by a physician or other provider for Medicare services billed under the Medicare Part B Physician Fee Schedule. This is good news if you are doc seeing patients every day, but if you happen to own a dialysis facility, or an access center that functions as an ASC, you are out of luck, as in its current state the grace period will not apply to the claims those facilities submit. Hospitals also find themselves in the same boat and, as you might imagine, they are none too happy about this minor nuance. Apparently the American Hospital Association is working hard on this issue, but I would not count on resolution prior to October 1.
Next, check out FAQs #3 and #5. CMS is attempting to make it clear that if the claim has a “valid” code, in most circumstances the grace period applies. (I say “most cases” because of the dirty little secret revealed in FAQ #7. More on that later.) A valid code, CMS points out, is a code selected from the appropriate “family of codes.” For example, E11 defines the type 2 Diabetes Mellitus family of codes. There are a boat load of codes that begin with E11, each with a total of 4, 5 or 6 characters. What CMS appears to be saying is if you send them a code for type 2 DM that has at least 4 characters, life will be good during the 12-month grace period. But if you send them E11, the claim will be denied. Just to make matters a little murkier, there are some 3-character codes that have no additional specificity beneath them. Of particular interest to the nephrologist is the new code for essential hypertension. That code is I10. When you look at a tabular list of the ICD-10 codes you will notice the next code after I10 is I11 (hypertensive heart disease). I11 is a code family with lots of “children” beneath it, therefore it is not a valid code, and if you use it CMS will reject your claim. I10 on the other hand is a valid 3-character code; use it and no problem. Clear as mud, right?
Falling from grace
Are there examples where a lack of specificity will lead to a claim rejection during the grace period? I am afraid the answer is yes. Apparently there are a number of Local and National Coverage Decisions (LCD and NCD respectively) that have been handed down through the years which demand specificity. FAQ #7 referenced above addresses this particular issue and it makes it clear that Medicare review contractors such as Medicare Administrative Contractors, the Recovery Auditors, the Zone Program Integrity Contractors, and the Supplemental Medical Review Contractor will require the same level of specificity in ICD-10 as they presently require for ICD-9. Note things like laterality are not possible in ICD-9 so the contractors will not hold your feet to the fire there, but short of that it is business as usual.
FAQs #10 and #11 raise additional concerns. Number 11 highlights the fact that the grace period applies only to Medicare and that “This Guidance does not apply to claims submitted for beneficiaries with Medicaid coverage, either primary or secondary.” Oddly, FAQ #10 states that in cases of a crossover claim, Medicaid can deny claims without a valid code. The implication is they will not reject the claim for lack of specificity which does not jive with FAQ #11, so your guess is as good as mine with respect to the crossover claims. Last but not least, FAQ #13 states the obvious; although CMS has issued this guidance for physician claims submitted to Medicare, Lord only knows what the commercial payers will do.
The good, the bad, and the ugly
At the end of the day, the grace period reminds me of something my father used to say, “it’s better than a sharp stick in the eye.” If nothing else it will provide a learning experience for docs and practices. When Medicare denies a claim, they will let you know if the reason for the denial was lack of specificity (due to an NCD or LCD) or if the code you submit was not a “valid” code. As for the bad, it is a bit troubling this applies to Medicare and not Medicaid. And the ugly? Most docs see a patient and render a diagnosis code but do not have a clue who the payer is. In those practices, the grace period offers no quarter as the doc must work towards the least common denominator so to speak and select the most specific code available for every patient they see.
I think many physicians have underestimated the pain this transition is going to bring. Most physicians are busy and frequently they wait until the last minute. (You know who you are.) 😉 This is truly one of those areas where an ounce of prevention is worth a pound of cure. Do yourself a favor, take that free training session your local hospital or medical association is offering. Listen carefully to your informed practice manager when he or she makes an ICD-10 suggestion. This is going to be a painful process, but your preparation will help ease the pain.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.




Leave a Reply