 Happy December everyone! I hope Thanksgiving was enjoyed by one and all, and that each of you has seen your last turkey sandwich for a while. Before you know it we will be ringing in the New Year, and what a year it will be. Some of you will face the Stage 2 meaningful use objectives, some will tackle the Stage 1 objectives, and others will file for a hardship exception, but each of you will experience the joy that is the looming ICD-10 transition. Okay, perhaps “joy” is a bit optimistic, but in the spirit of the holiday season, let’s take a closer look at next year’s code transition.
Happy December everyone! I hope Thanksgiving was enjoyed by one and all, and that each of you has seen your last turkey sandwich for a while. Before you know it we will be ringing in the New Year, and what a year it will be. Some of you will face the Stage 2 meaningful use objectives, some will tackle the Stage 1 objectives, and others will file for a hardship exception, but each of you will experience the joy that is the looming ICD-10 transition. Okay, perhaps “joy” is a bit optimistic, but in the spirit of the holiday season, let’s take a closer look at next year’s code transition.
ICD what?
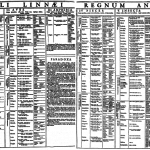
The international statistical classification of diseases and health-related problems (thankfully shortened to ICD) is a classification system created by the World Health Organization (WHO). ICD-10 is the tenth revision of this classification system. What many will find of interest is that ICD-10 has been in use around the world since its introduction in 1992. That’s right, ICD-10 is over 20 years old and it is used today by every industrialized nation except ours. Ironically, as we approach the U.S. adoption date for ICD-10, the WHO is putting the finishing touches on ICD-11.
Today we use the ICD-9 code set. ICD-9 was published in 1977, a year some of us spent in high school, but I digress. There are substantial differences between ICD-9 and ICD-10, not the least of which is the magnitude of the number of codes. In the U.S. we have expanded upon the WHO list and created Clinical Modifications of ICD, frequently referred to as ICD-CM. It is this latter group of codes you draw from when submitting a claim to a payer. I tend to think of those claims in very simplistic terms. When a provider delivers a medical service he or she documents that service in the patient’s medical record. Receiving reimbursement for the work performed requires submitting a claim to the entity responsible for paying for the service rendered. That claim contains several important pieces of information, not the least of which is a pair of codes. The Current Procedural Terminology code, or CPT code, tells the payer what you did during the encounter, and the ICD-9 code tells the payer why you did it.
The numbers (and letters)
When it comes to ICD codes, there are substantially more 10s than 9s. Depending on how you count, ICD-9 CM has about 14,000 diagnosis codes and around 4,000 procedural codes. On the other hand, ICD-10 CM arrives with over 68,000 diagnosis codes and over 72,000 procedural codes. Many providers have memorized specific ICD-9 codes through the years. The ICD-9 format makes this a trivial exercise as we are all capable of remembering 4 or 5 digit numbers, particularly when we see them several times each week. The ICD-10 framework will make this a bit more challenging. ICD-10 codes typically consist of 7 characters (numbers and letters). Character positions 1-3 identify the disease category, character 4 reflects the etiology of the disease, character 5 describes the affected body part, 6 defines severity of the illness and 7 is a placeholder which permits increasing the specificity of the description.
Technical vs. operational change
As nephrology and medicine continue the transition to the digital world, a number of technical changes must occur as adoption proceeds. Today, with rare exception, the claim that tells the payer what you did and why you did it moves from your office to the payer electronically. Last year, whether you knew it was happening or not, your billing platform went through a significant upgrade, frequently referred to as the 5010 transaction standard. This change was necessary to accommodate the movement of ICD-10 codes from your office to the payer. This year and next, the clinical systems you use (office- and hospital-based EHRs, dialysis information systems, etc.) are making the necessary technical changes to accommodate the I9 to I10 transition.
In my view, the technical changes are relatively easy compared with the operational challenges the typical nephrology practice will face. For example, consider that the codes should reflect what appears in the medical record on the date(s) of the encounter with the patient. This is true regardless of where that encounter took place. In my travels around the country over the past several years I never cease to be amazed by the diversity of work flow I see surrounding the creation of the claim. Sometime the doc handles everything, placing the CPT code and the ICD-9 code on the claim. On the other hand, I’ve seen situations where the doc creates the documentation and leaves the generation of codes to other members of the medical practice. Regardless of where you fall within this spectrum, it is extremely important to understand the relationship between your documentation and the diagnosis code will become even more important with ICD-10. The depth and breadth of ICD-10 creates the opportunity to become much more granular, but this granularity requires sufficient documentation.
October 1, 2014
The new codes take over in 303 days, or ten months as of yesterday for those of you keeping score. Seems like a lot of time, especially with everything else on our plates next year. But don’t short change this one. The 9 to 10 transition will impact everyone in your practice. If you have not already done so, begin thinking about how you translate medical documentation to CPT and ICD-9 codes in your practice today. Determine if this work flow will need to change as ICD-10 approaches. Encourage your providers and appropriate members of your billing staff to attend an ICD-10 documentation and coding class. Change is always accompanied by some degree of discomfort. Planning ahead for the ICD-10 transition will go a long way towards easing the pain for your practice.


Leave a Reply