
As if there wasn’t enough excitement from COVID-19, Medicare Advantage plans opening for dialysis patients, and additional new final regulations under the 21st Century Cures Act, CMS has dropped a new Final Rule that will have potentially large financial impact on many nephrology practices and dialysis facilities in numerous markets across the country.
Following more than a year of comment review and edits after the publication of the proposed rule last summer, on September 18, 2020, CMS and HHS revealed the Final Rule on the mandatory ESRD Treatment Choices (ETC) Model. The model will launch on January 1, 2021, and run through June 30, 2027.
The Final Rule on ETC is part of a 957-page document covering both a Radiation Oncology Model of Care and ETC, affecting reimbursement for nephrology practices and dialysis clinics alike. PRO TIP: Focus on reading pages 931 thru 956—that’s where the ETC action (the actual rule) is located. Most of the preamble and the responses to comments are of passing interest at best.
Here are some key things for nephrology practices to know:
Some practices are in and some are out. And CMS has already decided who those practices are. Using 306 US geographic regions (called Hospital Referral Regions), HHS has randomized 95 geographies to be included. These geographies include about 30% of ESRD Medicare beneficiaries (and exactly 35% of Acumen client practices). To find out if your practice is included, visit the CMS website where you can select from a lengthy list of ZIP Codes. If your ZIP Code is not on the list, CONGRATULATIONS! You can stop reading now. If your ZIP Code is on the list, then WELCOME, MY FRIEND, TO THE ETC MODEL!
If your practice’s ZIP Code has been selected, the ETC Model is mandatory. Unlike other Kidney Care Choices models, you have no choice in whether you and your practice participate or not (unless you decide to pack up and move your practice to an unaffected ZIP Code).
ETC is a grand experiment. CMS intends to collect data and compare the performance of included practices (called “participants”) to excluded practices over the coming 6 years in two broad areas: home dialysis and transplantation. Participants will be subject to financial incentives. Excluded practices receive no incentives and will be used as the control group to ascertain the effectiveness of the incentives in increasing home dialysis and transplantation rates.
There are two financial incentives for participants. The first is the Home Dialysis Payment Adjustment (HDPA) and the second is the Home Dialysis and Transplant Performance Assessment and Performance Payment Adjustment (simply called the PPA).
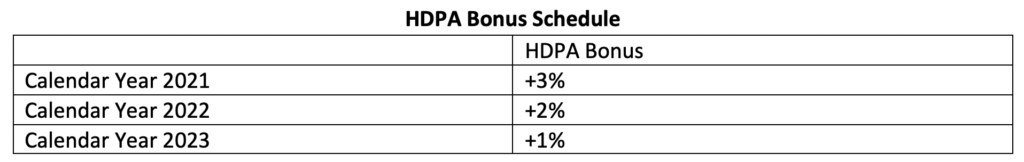
You don’t need to lose sleep over the HDPA. This adjustment is simple to understand and entirely positive for your practice. It’s all upside! For every home dialysis MCP claim paid by CMS (specifically for CPT codes 90965 and 90966) for patients who are at least 18 years of age, CMS will apply a bonus for the first three years of the ETC program. The size of the bonus decreases each year according to the following schedule:
You DO need to lose some sleep over the PPA! The PPA is a MUCH MORE COMPLEX animal with upside and downside adjustments that grow over time. And you will likely need a degree in calculus and a slide ruler to figure it all out. Let’s start with the end in mind. CMS intends to base the PPA on all of a nephrologist’s Medicare MCP claims (in-center and home) and make payment adjustments based on a new score called the Modality Performance Score (MPS). (More about the MPS in a moment.) And CMS has devised a complex calendar of 10 rolling 6-month periods called PPA Periods, each with an associated prior Benchmark Year and Measurement Year. (More about this calendar and those special years in a later blog post.) The first PPA Period starts on July 1, 2022, and the last PPA Period ends on June 30, 2027. In the table below are the adjustments for clinicians for each of the periods. (A similar separate set of scores and adjustments are applied to dialysis facilities in the selected ZIP Codes.)
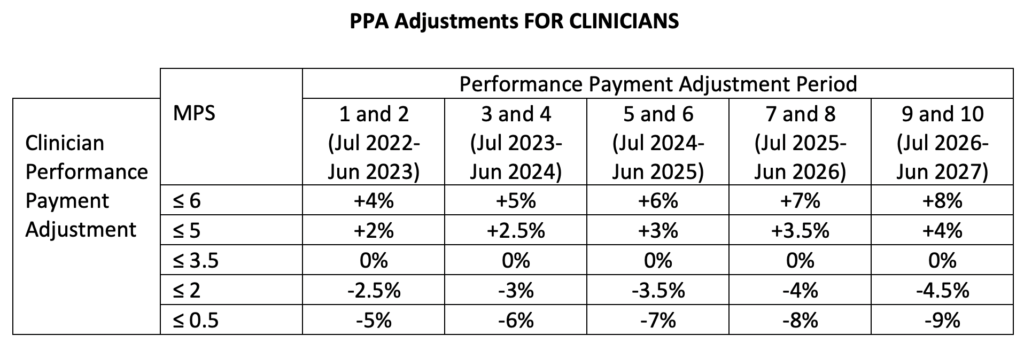
As you can see:
- The payment adjustments GROW over time.
- The payment adjustments are ASYMMETRIC (i.e. the magnitude of the maximal penalty is always greater than the magnitude of the maximal bonus).
- The whole program is based on the MPS.
Understanding and Maximizing the MPS is KEY. For purposes of this blog post, we are going to keep things high-level and strategic. In a subsequent post, we’ll work through the actual calculations CMS is going to be using for the MPS. (Bring your slide ruler.)
The MPS is a number from 0 to 6. It is derived from the clinician’s home dialysis rate (which counts for two thirds of the score) and the clinician’s transplant rate (which counts for one third of the score).
For both the home dialysis rate and the transplantation rate, there are two ways to put some MPS points on the board: the achievement benchmark and the improvement benchmark (whichever yields the higher point value for the practice).
For transplant, for example, take a glance at the following table:
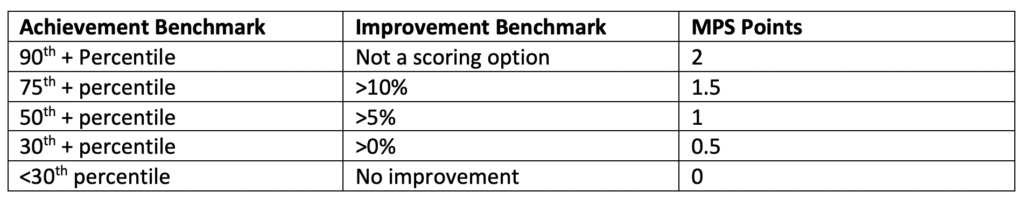
Let’s say that your practice scored in the 45th percentile for transplantation achievement compared to other participating practices. That can earn you 0.5 MPS points. (Not so good.) But let’s also say that your practice improvement for transplant rates compared to the corresponding benchmark year was a whopping 11%. That can earn you 1.5 MPS points. CMS will award the larger point value. In this case, you get to put 1.5 points up on the MPS leaderboard (reflecting your improvement).
Rinse and repeat for home therapy. But remember, multiply your home therapy points by 2 before adding them to your transplant points since home therapy (which counts for two thirds) is worth twice as much as transplant (which counts for one third) in the MPS score.
If you have made it this far, you are doing great! You’ve got the fundamentals of the ETC program down. But there are a few nagging details you will want to keep in mind.
CMS plans to EXCLUDE some patients from the PPA. Specifically, Medicare beneficiaries with any of the following characteristics will not figure into the calculations:
- Is not enrolled in Medicare part B
- Is enrolled in Medicare Advantage, a cost plan, or other Medicare managed care plan
- Does not reside in the United States
- Is younger than age 18
- Has elected hospice
- Is receiving dialysis for any acute kidney injury (AKI)
- Has a diagnosis of dementia
- Is residing in or receiving dialysis in a skilled nursing facility (SNF) or nursing facility
The home rate now includes in-center, self-care patients. However, such patients count for only half as much as patients who dialyze fully at home.
Transplantation rates are the trickiest part of the MPS. At a high level, the transplant rate takes into account patients on a transplant waitlist as well as those who receive living donor transplants (both pre-emptively and for ESRD). This topic is so complex that it deserves its own blog post, which we will be posting soon. The best news about this topic is that the Final Rule includes patients on transplant waitlists (which was not part of the proposed rule). And the ECT Model, in general, provides incentives for early transplant listing.
You and your practice will not need to submit any new data to CMS. CMS will be implementing the ETC Model using claims data from your practice (and from other practices and facilities where the patient is seen) as well as additional data from other sources like the Scientific Registry of Transplant Recipients (SRTR). So the administrative disruption of the program on nephrology practices is likely to be small.
Acumen is taking active steps to help you and your practice succeed. Specifically, we are developing new dashboards that will allow you to see the performance of your practice as it relates to home therapy and transplantation. And we are enhancing workflows to make it easy for you and your practice to review and document the data that are needed for these performance estimates. These tools will allow you to actively monitor the progress of your practice on these measures and take steps to intervene and improve. (These tools will obviously be helpful to practices that have been randomized to the ETC Model, but should be of general benefit to any practice looking to improve performance in the areas of home therapy and transplantation.)
There will be much more to come on the ETC Model. In the meantime, please reach out to us with questions and, especially, suggestions on how we can support you and your practice in this rapidly approaching era of ETC.
 Timothy McNamara, MD, MPH is Sr. Director of Clinical Health IT in FMCNA Medical Office, and serves as Acumen’s Medical Director. Dr. McNamara is a physician with an extensive health informatics background. He brings 26 years of experience in healthcare IT from work in both corporate and academic environments.
Timothy McNamara, MD, MPH is Sr. Director of Clinical Health IT in FMCNA Medical Office, and serves as Acumen’s Medical Director. Dr. McNamara is a physician with an extensive health informatics background. He brings 26 years of experience in healthcare IT from work in both corporate and academic environments.
Photo above by lan deng on Unsplash



Amanda Williams says
Good morning,
Our Martinsville, VA dialysis unit is in an SGR, however in reading over some additional information it appears we would not be subject to ETC because our MCP billing is done from a central billing office based out of Roanoke, VA. Could you confirm this or point me in the right direction?
Thanks
Timothy McNamara, MD, MPH says
Thanks for the question!
Our understanding is that CMMI intends to look at your practice zip code as recorded in Medicare’s Provider Enrollment, Chain, and Ownership System (PECOS) in order to determine if your practice is in the mandatory model. You may want to confirm the zip code on file for your practice in PECOS by visiting: https://pecos.cms.hhs.gov/pecos/login.do#headingLv1
Once you have the zip code confirmed, you can confirm whether it is part of the mandatory model by locating it in the long list of zip codes selected for participation at this web site:
https://innovation.cms.gov/innovation-models/esrd-treatment-choices-model
For reference, the exact language from the final rule (512.325.a) appears to be silent on this specific question. It says simply: “Selected participants. All Medicare-certified ESRD facilities and Medicare-enrolled Managing Clinicians located in a selected geographic area are required to participate in the ETC Model.”
Hope this provides some direction for your research!