
Last week we posted an introductory blog post regarding the ESRD Treatment Choices Final Rule that comes loaded with tricks (performance penalties) and treats (bonuses and incentives for home therapy and transplantation). This week, we spell out all of the scary details to help guide you through the hay-bale maze toward ETC success.
As you will recall, CMS has randomized approximately 30% of nephrology practices nationwide to be mandatory participants in this new program that starts soon (January 1, 2021) and runs through June 30, 2027.
Participant practices will receive financial incentives intended to increase transplantation rates and home dialysis rates for ESRD Medicare beneficiaries. There are two incentives:
- HDPA (Home Dialysis Payment Adjustment) provides a bonus on MCP payments for Home Dialysis (specifically for CPT codes 90965 and 90966) for the first three years of the program…3% bonus for calendar year 2021, 2% bonus for 2022, and 1% bonus for 2023.
- PPA (short for Home Dialysis and Transplant Performance Assessment and Performance Payment Adjustment) is a much more complicated adjustment, with up-side potential and down-side risk that will both grow in magnitude throughout the course of the ETC program.
The PPA is the focus of today’s blog. So, get out your slide ruler, protractor, pocket-protector, and propellor-hat (the perfect ETC Halloween costume) as we dig into the details.
The calendar
The PPA relies on a calendar of rolling 6-month time periods
each with an associated Benchmark MY (Benchmark Measurement Year), a MY
(Measurement Year) and a PPA Period. All three are separated by a 6 month
“buffer” interval). There are 10 PPA Periods in total for the ETC program.
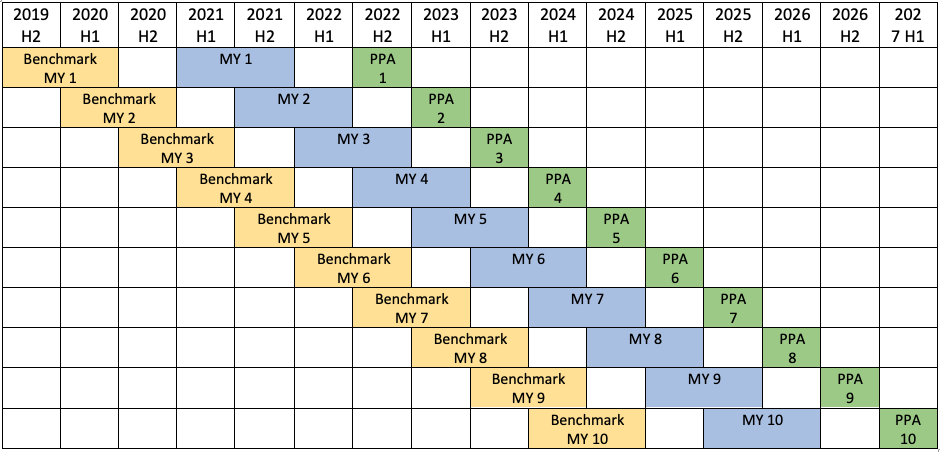
As an example, let’s take a close look at the first PPA Period, which is the second half of 2022. This is the first time that CMS will adjust all Medicare MCP claims (for both in-center and home patients). CMS is going to look back and calculate home dialysis and transplantation rates for each participating practice in the associated Measurement Year. CMS will also look back to the corresponding Benchmark Measurement Year to calculate 1) achievement benchmarks by evaluating home and transplant rates for other practices in the geographic comparison group (practices not participating in ETC), and 2) practice-specific improvement rates by comparing the benchmark measurement year and the measurement year.
These calculations are the basis for the all-important Modality Performance Score (MPS). As outlined in the prior blog post, the MPS is a number from 0 to 6. It is derived from the clinician’s home dialysis rate (which counts for two thirds of the score) and the clinician’s transplant rate (which counts for one third of the score). And this MPS is the magic number that sets the payment adjustment (again described in detail in a table in the prior blog).
Let’s look at the home dialysis rate, which is relatively straightforward. Then we’ll spend some time on the transplant rate.
The home dialysis rate
CMS calculates the home dialysis rate based on a denominator equal to the practice’s number of beneficiary years. (To calculate the beneficiary years, take the number of MCP claims for year, remove any claims for patients with exclusions per the previous blog, and divide by 12.) The numerator is the total number of MCP claims submitted for home therapy plus half the number of MCP claims submitted for in-center self-care, divided by 12.
The transplant rate
For the transplant rate, the calculation gets a lot trickier. CMS is going to consider three key items:
- The waitlist rate for patients on dialysis (Note: the inclusion of waitlist rates was a major change from the Proposed Rule!)
- The living donor transplant rate for patients on dialysis
- The pre-emptive living donor transplant rate
CMS calculates the transplant rate as the SUM of:
- The transplant waitlist rate, and
- The living donor transplant rate
For the transplant waitlist rate, the denominator is “the total dialysis treatment beneficiary years for attributed ESRD Beneficiaries during the MY.” Specifically, that means CMS will count the number of months when an attributed beneficiary received maintenance dialysis at home or in a center (12 beneficiary months equaling one beneficiary year). These months are identified by claims for CPT codes 90957, 90958, 90959, 90960, 90961, 90962, 90965, or 90966. IMPORTANTLY, CMS will exclude from the denominator any claims for beneficiaries who were 75 years or older at any point in the month.
The numerator is simply the total number of beneficiary years for which attributed ESRD beneficiaries were on the kidney transplant waitlist. CMS intends to use records from the SRTR (Scientific Registry of Transplant Recipients) as the “source of truth” to determine if a beneficiary is on a waitlist.
For the living donor transplant rate, the denominator is the SUM of:
- “The total dialysis treatment beneficiary years for attributed ESRD Beneficiaries during the MY”—using the method described above, and
- “The total pre-emptive LDT beneficiary years for attributed beneficiaries during the MY.” This number is calculated from the number of months during which a pre-emptive LDT beneficiary is attributed to a clinician from the beginning of the MY up to and including the month of living donor transplant. CMS will use the SRTR and Medicare claims data to identify patients who received a living donor transplant.
And the numerator is the SUM of:
- The total number of attributed beneficiary years for LDT beneficiaries during the MY. This number includes the number of months from the beginning of the MY up to and including the month of transplant, and
- The total number of attributed beneficiary years for pre-emptive LDT beneficiaries during the MY. This number also includes the number of months from the beginning of the MY up to and including the month of transplant. (Both of the numbers in this numerator are based on data from the SRTR and Medicare claims data.)
One other important fact: CMS will ‘risk adjust’ the transplant waitlist rate based on beneficiary age with separate coefficients for the following age categories. The details of this risk adjustment are a bit vague but they will be based on a comparison of each ETC participant’s patients to a national age distribution of beneficiaries who are not excluded.
- Age 18 to 55
- Age 56 to 70
- Age 71 to 74
The take-aways
So, there you have it! Not quite a bone-chilling terror, but a bit of a fright-fest all the same. Here are the key take-aways (in addition to the items in the prior blog post):
- For ETC participants, achievement (and/or improvement) in home dialysis rates and transplantation rates are critical in order to avoid payment reductions and open opportunities for payment increases in MCP starting in July 2022
- Benchmark rates for your practice have already been determined. And the first measurement year starts soon (January 2021)
- Home therapy rates are weighted twice as much as transplant rates in determining MPS (modality performance scores)
- Transplant rates take into account transplant waitlisting as well as pre-emptive living donor transplantation and living donor transplantation for ESRD
As described in the prior blog post, Acumen is taking active steps to help you and your practice succeed. Specifically, we are developing new dashboard components that will enable you to peer through the swirling fog and see the performance of your practice lit up from the light of a bright full moon. And we are enhancing workflows to make it easier for you and your practice to review and document the data that are needed for these performance estimates.
We are in this together! And we hope that you will reach out to us with questions and, especially, suggestions on how we can support you and your practice (and keep the ETC scares at bay).
 Timothy McNamara, MD, MPH is Sr. Director of Clinical Health IT in FMCNA Medical Office, and serves as Acumen’s Medical Director. Dr. McNamara is a physician with an extensive health informatics background. He brings 26 years of experience in healthcare IT from work in both corporate and academic environments.
Timothy McNamara, MD, MPH is Sr. Director of Clinical Health IT in FMCNA Medical Office, and serves as Acumen’s Medical Director. Dr. McNamara is a physician with an extensive health informatics background. He brings 26 years of experience in healthcare IT from work in both corporate and academic environments.
Photo by Neven Krcmarek on Unsplash



Leave a Reply