I spend a lot of time talking to nephrologists about electronic health records. Some of these docs have used an EHR for over 15 years; others have been using paper charts for 30 years and are just preparing to dip their toes in the water. A common discussion point with providers of both vintages is electronic prescribing. eRx is a hot topic these days, both as a fundamental component of the meaningful use incentive program and as the source of the first CMS pay-for-reporting penalty, which many nephrologists are facing this year.
CMS programs aside, what is the upside to sending a prescription electronically?
Everyone knows that although it is impossible to complete an electronic script faster than you can scratch one out on a paper pad, legibility is a classic concern, appropriately raised as part of this debate. In addition, some will say the clinical decision support (CDS) offered by drug-drug and drug-allergy interactions brings an intelligence to the prescribing process not readily available outside the eRx realm. Who has time to thumb through the mind-numbing volume of clutter contained within a PDR for example? Of course anyone who has used an eRx tool recognizes that the value of CDS in this venue is substantially marginalized by alert fatigue. Finally, prescribing electronically provides the added benefit of formulary restrictions, which when used properly avoid an all too common scenario. For example, I write a script for Lipitor, hand it to the patient, then receive a call from my office three hours later when the patient is at the pharmacy and finds that Lipitor is not on his drug plan’s formulary.
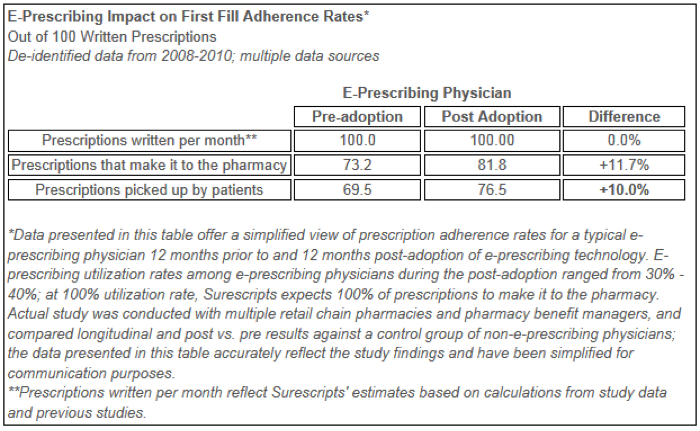
Regardless of whether you feel any of the above scenarios make the case for embracing eRx, I recently came across an announcement by Surescripts which confirms something I had heard in the past. It turns out that patients are more likely to fill their prescriptions if you send them electronically. Think about that for a minute. Examining a very large number of providers and prescriptions, the folks at Surescripts studied fill rates for handwritten prescriptions, then looked at those rates after docs began e-prescribing. I have copied the pertinent table below from the Surescripts reference:
In this large cohort of patients and providers, simply switching from paper to eRx resulted in a fairly sizable difference in the number of prescriptions patients actually filled. What’s more, this change occurred in spite of the fact that the e-prescribers used the eRx tool less than half of the time. Granted, these were not likely to be ESRD patients, but imagine the impact if these findings translate to that population of patients. It’s certainly food for thought.
The next time you find yourself frustrated with eRx because your Internet connection is slow or the GUI is archaic and lacks a dose of user-centered design or alert fatigue is driving you nuts, think about the impact you are having on patient compliance. True, the study above does not prove patients are taking those meds, but you have to bring them home before you can swallow them.

Leave a Reply