 When I was much younger, one of my favorite treats was a family trip to the local ice cream parlor. There was a Baskin-Robbins in the neighborhood and I still remember the excitement and amazement surrounding all of the available choices. How could there possibly be 31 flavors of ice cream? I’d stand on my toes and peer through the glass at all the buckets, trying to decide what flavor to choose. Fast forward more years than I care to admit. I still like ice cream and for some reason the 31 flavors image came roaring back when I was exploring meaningful use data from 2011. I know it’s a reach but bear with me.
When I was much younger, one of my favorite treats was a family trip to the local ice cream parlor. There was a Baskin-Robbins in the neighborhood and I still remember the excitement and amazement surrounding all of the available choices. How could there possibly be 31 flavors of ice cream? I’d stand on my toes and peer through the glass at all the buckets, trying to decide what flavor to choose. Fast forward more years than I care to admit. I still like ice cream and for some reason the 31 flavors image came roaring back when I was exploring meaningful use data from 2011. I know it’s a reach but bear with me.
Our Federal government maintains a very handy website that contains all sorts of interesting information. If you dig deep enough you will find a compilation of meaningful use related data, including information from the ONC, CMS and the CHPL (Certified Health IT Products List) rendered in a useful spreadsheet format. Using some Excel magic, one can find interesting tidbits buried in this sea of data. For example, almost 700 nephrologists successfully attested to meaningful use in 2011. Depending on whose figures you choose to use, that’s roughly ten percent of the nephrologists in this country.
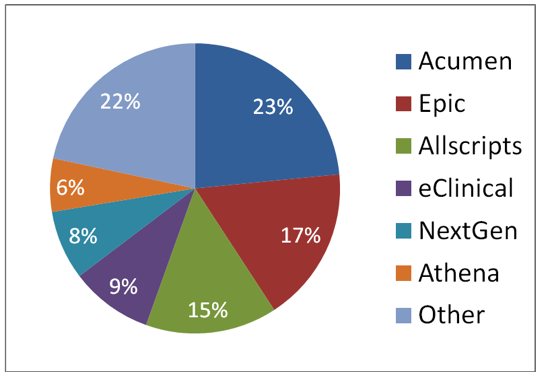
Of further interest, those nephrologists used 35 different EHRs to accomplish this task. (Okay, it’s not 31 flavors but its darn close.) Similar to the ice cream parlor experience, some EHRs were consumed frequently, others only rarely so. There are several EHRs on this list that were used by a single nephrologist and others that were used by only a handful of docs. Check out the pie chart below which displays the EHRs most commonly used by nephrologists who demonstrated meaningful use in 2011:
I learned a couple of things during this exercise worth noting. First, the three most commonly used applications accounted for over half of the meaningful use attestations by nephrologists in 2011. Second, in spite of spending the past four years in this industry, there are many EHRs on this list of 35 that I have never heard of. Finally, I was a little surprised by the size of Epic’s slice of the nephrology pie.
Epic is the premier hospital-based EHR in the land these days. In communities where an EHR has been installed within a hospital, the vast majority of employed physicians are compelled to use the ambulatory version of the vendor’s EHR. This is particularly true in areas of the country where vertically integrated health systems exist; Kaiser is perhaps the best example. Some community physicians have also felt the pull towards utilizing an EHR chosen by a regional hospital. However, as the nation’s infrastructure for data sharing matures over the next few years, I think we will see fewer providers selecting EHRs based upon a local hospital’s decision.
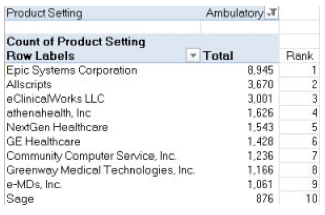
As I was putting together this information, I came across this related graphic compiled by an anonymous commenter on the HISTalk site:
The table displays data from the same source I cite above but examines the entire universe of eligible professionals who demonstrated meaningful use last year. Epic dominates this list, again likely representing a large contingent of employed physicians across the country. I think the large Epic presence here may also be explained by the large number of primary care providers who qualify for this program via the Medicaid. Those providers will receive their year 1 incentive simply by attesting to the fact that they are implementing a certified EHR. Within this context, Epic’s position in the general market is not surprising, but I would have guessed their slice of the nephrology pie would have been smaller.
As 2012 progresses, the slices of the nephrology pie are bound to change. The number of flavors will likely increase in the short term before ultimately declining. Food for thought the next time you find yourself contemplating a scoop of black walnut vs. chocolate chip. Bon appetit!

Jim Robertson says
Learnng to count (dialysis rounding and meaningful use):
My group of 4 nephrologists/2 extenders is struggling to decide whether to include dialysis rounding in our meaningful use quest. I went to grade school in the era where “new math” was a buzzword, and it seems I’m facing new “arithmetic” more than 50 years later. For example:
1. Do I count all the visits on one patient during a quarter as ONE encounter?
2. Do the G-codes I use for billing dialysis encounters even count AT ALL (I remember being told back in 2010 that dialysis visit billing codes weren’t among those that qualified for meaningful use attestation in the numerator, but that they DID qualify in establishing the total number of visits I make during the reporting period (I may be confused here; perhaps it’s the e-Prescribing initiative where the dialysis visit billing code excludes qualification)
3. Let’s assume that all dialysis facility encounters I have with one of my patients during the reporting period are considered one unique encounter. When do I have to reach the bar for individual measures; e.g., must the problem list be in place the first time I see the patient, or can I have it in place the LAST time I see him and still qualify.
4. What happens to visits made by my extender (we use a family practice MD and a Nurse Practitioner). Are their visits with this same patient during the quarter counted as ONE encounter? How about the situation where I do the comprehensive visit and the extender does all 3 limited visits? Given that it’s much harder to make a limited visit encounter record meet the “15 measures” threshold, will my group be punished for using extenders whose limited visits therefore aren’t “meaningful use” certifiable?
5. If we decide we can exclude dialysis rounding encounters from our meaningful use qualification (with almost 400 ESRD patients in our practice my guess is we’ll not be able to take this path, but let’s imagine it’s possible), can we avoid reporting the activities of our extenders altogether? (The only thing they do for us is rounding on in-center dialysis patients).
6. Does the “new arithmetic” change for Phase 2 attestation?
Terry Ketchersid, Vice President and Medical Officer at HITSG says
Jim, I like the new math analogy and as I type from the Dialysis Conference in San Antonio, the Texas 2 Step comes to mind. As nephrologists, our first step is deciding whether or not at least half of our patient encounters take place in a venue of care equipped with a certified EHR. All hospital encounters are excluded from this calculation, but everything else is in including office, dialysis and even access center patient encounters. For this first step we are counting every encounter. If you see the HD patients 4 times each month that counts as 4 encounters. With regards to your mid-level providers, CMS tells us you can go one of three ways; you can count them as encounters on your side of the ledger (not sure why you would), or they can count the encounters for themselves if they qualify via the Medicaid path (very rare), or you both could count them (again, not sure why you would). So for the first step, most nephrologist with mid-levels are not counting the mid-level HD encounters.
For most nephrologists the dialysis encounters make up a very large percentage of the encounters in step one. A common confusion I see today is nephrologists believe they have a choice here. In fact you either meet step one or you are not eligible for the meaningful use incentive. Further, once your determine that half of your encounters do occur in a location(s) equipped with a certified EHR, you must report the patients seen in those locations, that is to say there is not an option to include or exclude the dialysis encounters. If you bring certifed EHR into a dialysis facility you must include those patients.
The second step in this dance assumes you are eligible and are ready to report. Most (but not all) of the objectives with a target threshold (like the problem list objective) examine something called a “unique patient encounter”. If you see a dialysis patient 4 times per month during the 90 day year 1 reporting period, that patient is counted one time in the problem list objective denominator. To be counted in the numerator for that objective, on at least one of those 12 encounters, the patient must have had at least one problem on their problem list (or a record they have no problems which obviously never occurs in a dialysis facility). Note also anyone can put the problem on the problem list (like one of your mid-levels for example) and you still receive credit.
I think your confusion about dialysis encounters not being included is indeed related to the e-precribing program-they are specifically excluded from the incentive, although this year you can use them to avoid the penalty…just to add to the confusion.
Finally, the proposed rule for the stage 2 objectives was published last week and yes, the new arithmetic of the Texas 2 Step described above remains in place.
I hope this helps and many thanks for your thoughtful comment.
Terry
Jim Robertson says
Now I’m wondering if mine wasn’t a “new math” question but rather a grammar question (my mom was a 90 pound wonder of a high school English teacher).
The issue may be different from what i suspected. Currently, the dialysis centers where I work are not “equipped” with a Certified EHR. They all DO have rudimentary web-based EMRs that permit me to document my visits in a manner that permits the facility staff to read my encounter notes. I didn’t realize that I could make the universe of my outpatient encounters solely those that take place in my office (where presumably I’ll have a certified EHR installed), but be excused from using it to document my dialysis rounding altogether!
That may be the best of both worlds – at least for now.
Terry Ketchersid, Vice President and Medical Officer at HITSG says
Jim, I could have used your mom’s help as I may not have been clear before. The provider actually is not able to exclude the dialysis encounters at will. The first step is determining where your encounters a performed. If over half of your encounters occur in the office and the certified EHR is in the office alone (not in the dialysis unit), you would be eligible for the program and you would report the office encounters. If over half of your encounters occur outside the office, but the office is the only location with a certified EHR, you are not eligible for the incentive. If the encounters that take place in the office and in the dialysis facility account for over half of your encounters (most common scenario for a nephrologist) and you bring your office based certified EHR into the dialysis unit, you are eligible and you would report the office and dialysis encounters for meaningful use. I do not believe the architects of this program had the practice of nephrology in mind when they put this framework together.
Jim Robertson says
(and yet two MORE wrinkles)
One of the clinics where I round is owned by an LDO. I’m the Medical Director, and I sublet space there to conduct a CKD clinic. Once I have a “certified” EHR that I’m using for my office practice, would using it for my CKD practice in that building constitute “installation of a certified EHR” at that physical location (the LDO dialysis center), given that I’d be billing for the CKD visits as though I’m “at” a remote outpost of my office?
The other issue is that my partnership holds a contract with an HMO through which we provide their local medical center’s nephrology care (hospital consultation and follow-up, CKD outpatient clinic staffing at their facility, and care of their members with ESRD at the dialysis clinics where we practice locally. We’re compensated for the CKD clinic care and hospital care on a constant stipend basis, but paid at commercial rates for their non-Medicare ESRD patients and at Medicare rates for their Medicare ESRD patients (those payments come from the HMO, not directly from Medcare. Is there anything in the HiTECH Act stimulus provisions that addresses whether we need to include these patients when we do our “50% rule” calculations?
Terry Ketchersid, Vice President and Medical Officer at HITSG says
A couple of points related to the wrinkles. The first is the meaningful use framework is payer agonisitc and it is not tied to billing. Second the phrase “equipped with Certified technology” has been interpreted by CMS in a way that provides broad utiliazation (at least for the Stage 1 objectives). If you can log into your certified EHR from within the dialysis facility that would qualify. Interestingly they have also permitted users to capture data in a secondary location (like a dialysis clinic) then enter it into the certified EHR at another location (like in your office). This defeats the purpose from my perspective (hard to deliver real time clinical decision support if you enter the data after the fact for example) and it looks like this opportunity will go away in Stage 2, but it exisits today. Hope this helps.
Jim Robertson says
I’m beginning to understand how Bill Clinton could say “it depends on what the meaning of the word ‘is’ is. My take on the visit counting from what you wrote above was that the certified EHR must be the vessel in which we RECORD all our dialyis visits, not just that the certified EHR is available. So, if we’re reporting 4 visits, they all must be recorded in the certified EHR, and if we do 4 visits per month, all 12 encounters in a quarter will be counted in the denominator of the total number of encounters, and if we choose to do the monthly assessment notes in the certified EHR but the limited visits on paper or in the dialysis facility’s non-certified electronic record, we’ll be well under the 50% rule for establishing meaningful use.
Sorry to be so dense and so persistent, but I’m hearing widely different interpretations of this from people who are already attesting, and I want to make sure I get it right.
The obvious issue here is that completing an encounter in every certified EHR I’ve ever seen is a lot more complex than the “limited visit” notes that many nephrologists are accustomed to recording (often not much more than activating a checkbox that doesn’t say much more than “Kilroy was here”).
Thanks again for your insight.
Terry Ketchersid, Vice President and Medical Officer at HITSG says
Yes this is indeed more complex than it should be. To start with nothing in the meaningful use framework requires documenting an encounter. This of course is counter intuitive from the doc’s perspective as one would imagine meaningful use starts with the progress note (or MCP note in the dialysis facility). I am devoting time at a number of venues around the country to try to get the word out. Any chance you will be at the RPA meeting in DC this month? That’s my next scheduled public presentation about meaningful use. In the interim, take a look at tomorrows blog post. Also look at these FAQs from the CMS web site:
https://questions.cms.hhs.gov/app/answers/detail/a_id/10664
https://questions.cms.hhs.gov/app/answers/detail/a_id/10592/p/21%2C26%2C1058
https://questions.cms.hhs.gov/app/answers/detail/a_id/10466