
In a year filled with new regulations, new rules, new financial models, new viruses, and new ways of interacting remotely with patients, New Year’s Day will bring one final present: a package of new guidelines for E/M coding. So, let’s welcome in 2021 with a quick review of the new E/M coding system that CMS has planned for office practices.
Since the 1990s, US physicians have been billing for Evaluation and Management Services based on three-and-a-half key items: history, exam, medical decision making (MDM), and sometimes, in selected situations, time (for example, when counseling and coordination of care constitute more than 50% of the encounter, but only for face-to-face time with the patient). (Our sisters and brothers in other developed countries have looked on and said, ”WHAT?!?! You’ve got to be kidding!”) Recognizing this burden, in 2018, CMS launched the “Patients Over Paperwork” initiative to “cut the red tape.” And three years later, at the stroke of midnight on January 1, 2021, the baby will be born.
The fundamental difference between E/M 2021 and the iterations it replaces is that time and MDM are now the drivers for coding. Performance and documentation of history and exam are only required as medically appropriate. What this means is that the complex rules for counting the elements in an HPI, the number of systems reviewed in the ROS, and the number of body areas/organ systems examined go away. Instead, providers are given a choice on any individual office encounter to code based either on time spent or MDM.
One big caution: The new E/M 2021 changes only apply to office/outpatient encounters. E/M services provided in hospital, ED, nursing facility, etc. are NOT affected.
For E/M 2021, CMS retains the familiar “new patient” and “established patient” codes (with one exception…99201 “New Patient—Problem Focused” is being retired). With a little help from its friends at the AMA (the trademark holder for CPT Codes), CMS has re-defined the remaining office codes 99202-99205 and 99211-99215.
First, let’s take a close look at TIME
If you choose to code based on time, here are the 2021 definitions:
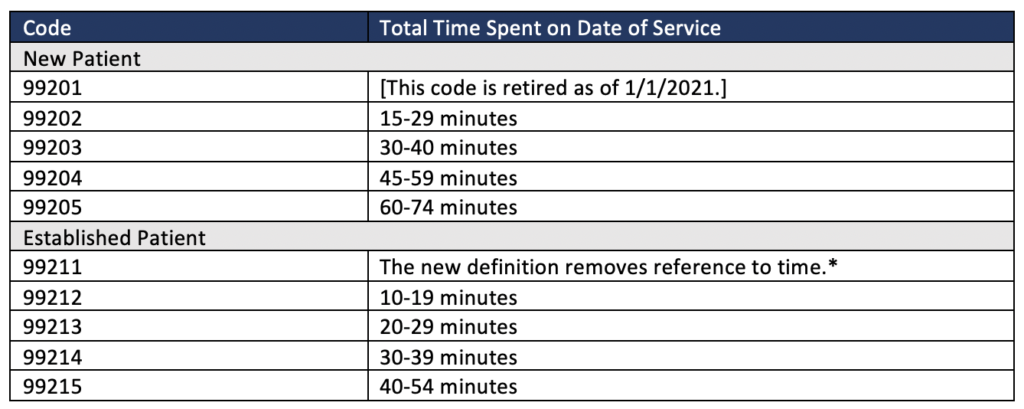
*99211 is newly defined as “Office or other outpatient visit for the evaluation and management of an established patient, that may not require the presence of a physician or other qualified health care professional. Usually the presenting problem(s) are minimal.”
A big change with E/M 2021 is that the total time spent by the provider includes both face-to-face AND non-face-to-face time spent on the date of service. And time-based coding can be used whether or not counseling and/or coordination of care dominate the service. Specifically, the new time-based coding may include time for the following activities:
- Preparing to see the patient (i.e. reviewing the chart or tests)
- Obtaining and/or reviewing separately obtained history
- Performing a medically necessary appropriate examination and/or evaluation
- Counseling and educating the patient/family/caregiver
- Referrals or discussion with other providers
- Documenting the clinical encounter
- Placing orders
- Writing prescriptions
- Reviewing results (on the same day of service)
- Care coordination that is not separately reported
A few important caveats regarding time-based coding:
- Clinic staff time (like the time to check in the patient and collect vitals) may not be included.
- If two qualified healthcare professionals (i.e. a physician and nurse practitioner) see the same patient together, only one can bill for the overlapped time.
- The “midpoint” and “threshold” times used in previous E/M guidelines go away. The new 2021 definitions give exact time ranges.
- For prolonged services (beyond the limits of 99205 and 99215) a new code temporarily called +99XXX will be available. Providers will be able to use +99XXX once for each 15 minutes beyond the primary service time (only for activities provided on the day of service).
- Currently there are conflicts between AMA (who creates CPT codes) and CMS regarding codes 99358 and 99359 (intended by AMA to cover prolonged services on a day other than the day of service). CMS has indicated that these codes will NOT be payable in association with E/M coding in 2021. Look for ongoing changes and evolution on this topic.
Now, let’s examine MDM
For MDM, AMA has closely examined the CMS “Table of Risk” and supplemented it with additional information from contractor guidelines and its own definitions and examples to create a single one-page (very small print) table that you should ABSOLUTELY download and print. See the table here.
Effectively, the level of MDM is broken into 4 categories:
- Straightforward (99202 and 99212)
- Low (99203 and 99213)
- Moderate (99204 and 99214)
- High (99205 and 99215)
(AMA provides an additional code—99211 described above—where MDM is not applicable.)
And, AMA associates each level with three Elements of Medical Decision Making (the three major columns in the table).
- Number and Complexity of Problems Addressed
- Amount and/or Complexity of Data to be Reviewed and Analyzed
- Risk of Complications and/or Morbidity or Mortality of Patient Management
To determine a code for a given encounter, find a row where at least two of the three elements are met.
In addition to reviewing the table, it is critical to understand the AMA’s definitions of the terms that appear in the table. The AMA has published a detailed document outlining the 2021 changes to office E/M coding. Three pages of definitions start on page 3.
How is Acumen 2.0 responding to these changes?
Early in January 2021, Acumen will be pushing out an update to 2.0 that incorporates the new E/M definitions. This update will affect relevant SmartSets and the Wrap-Up activity. It will also provide a new “Level of Service” calculating tool accessible from the wand icon below.
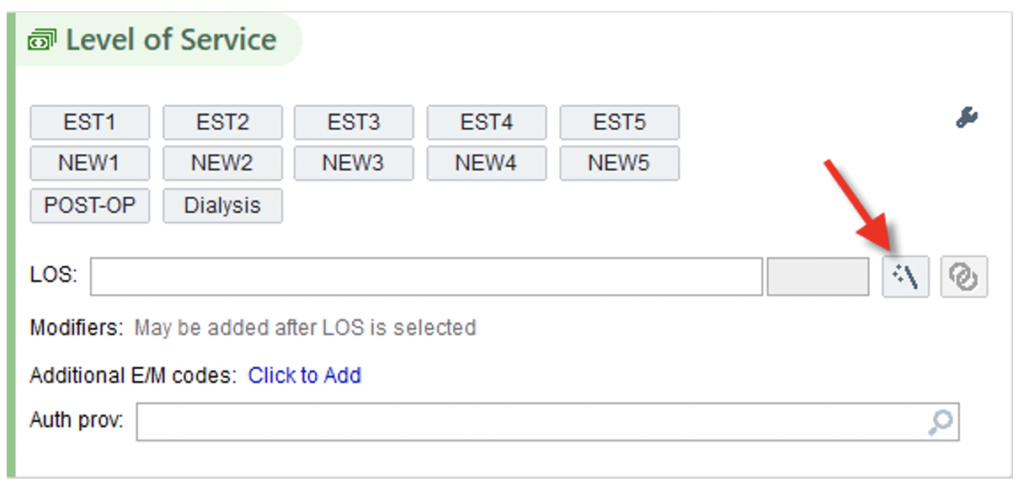
The new calculating tool will automatically suggest an E/M code for medical decision making based on chart documentation (including things like diagnoses and orders) and display the criteria that contribute to each level of service. Of course, users can change these suggestions as needed. It will also allow users to enter the total time they spent on the visit and it will then calculate the relevant service code.
For E/M coding for the first few days of 2021, providers can continue to select the same buttons as 2020, but the new definitions described above should determine which code providers select. Note “NEW1”—99201—should NOT be selected after December 31, 2020.
So Happy New Year and Happy Coding! Break out the champagne and the Hoppin’ John. And let’s hope that Uncle Sam’s plan to decrease administrative burden and paperwork for office visits brings some welcome relief in 2021!
 Timothy McNamara, MD, MPH is Sr. Director of Clinical Health IT in FMCNA Medical Office, and serves as Acumen’s Medical Director. Dr. McNamara is a physician with an extensive health informatics background. He brings 26 years of experience in healthcare IT from work in both corporate and academic environments.
Timothy McNamara, MD, MPH is Sr. Director of Clinical Health IT in FMCNA Medical Office, and serves as Acumen’s Medical Director. Dr. McNamara is a physician with an extensive health informatics background. He brings 26 years of experience in healthcare IT from work in both corporate and academic environments.
Photo from canstockphoto.com.



Leave a Reply