 My nights lately have consisted of rocking a sweet baby to sleep and binge watching episodes of Lost. WARNING – spoiler alert ahead for those late to the Lost party! I’m currently on the season where one of the main characters John Locke dies. Just when viewers are finally getting used to the somewhat mysterious character, he meets his demise.
My nights lately have consisted of rocking a sweet baby to sleep and binge watching episodes of Lost. WARNING – spoiler alert ahead for those late to the Lost party! I’m currently on the season where one of the main characters John Locke dies. Just when viewers are finally getting used to the somewhat mysterious character, he meets his demise.
However, if I’ve learned anything from Hollywood, whenever a main character suddenly disappears, you should always expect there’s more to come (Terminator, anyone?). In the case of the unfortunate John Locke, he comes back as a scary smoke monster.
What does the TV show Lost have to do with Meaningful Use you may ask? Well, for one, they both keep you on your feet with the constant change of events. Secondly, just when you think that something (or someone) is finally gone, it (or he) somehow resurfaces.
#SomethingBetter
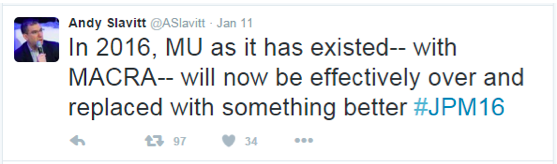
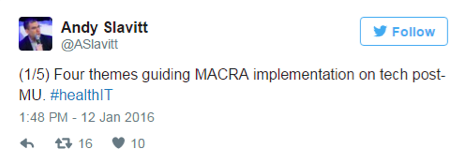
Last Monday, CMS acting administrator, Andy Slavitt, announced that “the Meaningful Use program as it has existed will now be effectively over and replaced with something better.”
He went on to say how CMS was in the process of putting providers back in the driver’s seat by allowing EHR technology to be designed around “individual practice needs, not the needs of the government.”
“We have to get the hearts and minds of the physicians back,” he said. “I think we lost them.”
In a panel discussion following the announcement, Slavitt noted that CMS is taking an “outside-in” approach to design the MU portion of MIPs by collaborating with groups like the AMA and with physicians directly.
“The stakes are high for this program,” Slavitt said. “As any physician will tell you, physician burden and frustration levels are real. Programs designed to improve often distract. Done poorly, measures are divorced from how physicians practice and add to the cynicism that the people who build these programs just don’t get it.”
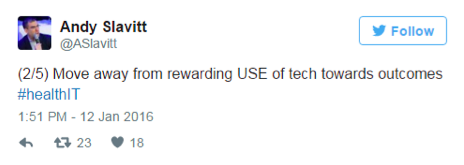
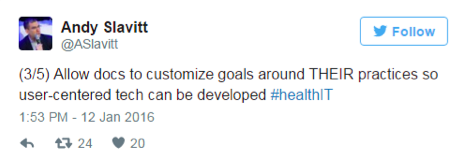
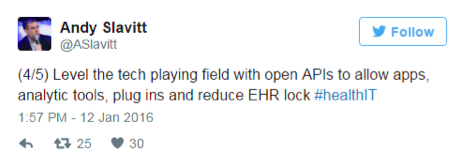
Although he didn’t give a lot of details on the changes we can expect to see in the next few months, he did leave a few clues via Twitter.
“I’ll Be Back”
Upon first hearing the news, my happy ears thought that the MU program will be blown to smithereens by the end of this year. I was not alone in that assumption. Immediately after the announcement, reputable industry leaders started applauding the end of MU by stating that “meaningful use ends in 2016” or “meaningful use is dead.”
However, after the excitement faded, the skeptic in me started to emerge. How can CMS just end MU like that? MU has been a main character for years and now it’s just gone? There was no talk about the 209,000 physicians who are taking a MPFS pay cut this year, or the countless number of physicians who are paying back MU dollars due to failing a nearly impossible-to-pass audit. Also, what does Slavitt mean by “something better”? Who gets to determine what’s “better”?
With so many unanswered questions, there’s obviously a lot to this story that still needs to unfold.
Here are a few reasons to believe that Meaningful Use will evolve rather than die.
- Congressional action
The Meaningful Use program was written into law under the HITECH act, which is part of the 2009 American Recovery and Reinvestment Act (ARRA). As with most laws, if it needs to be changed, there must be congressional action.
- MACRA and MIPs
We knew that the stand-alone MU program was set to go away and in its place will be the new Merit-Based Incentive Payment System (MIPS), as part of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). MACRA will sunset the three existing reporting programs and combine them into a single program. Part of the MIPs program will require providers to demonstrate MU, which will make up 25 out of the possible 100 merit points. Killing MU would mean reconfiguring how merit points would work. Instead, CMS will most likely keep the points system intact and redefine what MU means. This could be good or this could be bad.
Could CMS potentially make the MU component of MIPs more difficult to achieve? We have seen them take complicated to a whole new level in the past. Rather than rewarding physicians for using technology, MIPS will pay providers on using it towards improving their outcomes. As of now, we aren’t sure which part will be easier.
- The hospitals
Naomi Levinthal, senior consultant with The Advisory Board, points out that MIPs will only affect individual providers, not hospitals. For those hospitalists, does that mean staying course with the current Meaningful Use program even after 2016?
- The money
Some eligible hospitals and providers are still expecting an incentive payment. If there is no more MU, where will the billions of dollars remaining from the HITECH Act go?
- New administration
It’s possibile that the timing of the MIPs release and a newly elected administration could put all pending regulations on hold.
If CMS doesn’t quickly issue proposed regulations for the new plan, they may find themselves in a waiting game. This could cause a problem as 2017 will be the surveillance year for the first 2019 MIPs payment year.
Next Steps
Don’t burn those Meaningful Use training guides just yet! Although Slavitt stated that MU is “effectively over” and “something better” will be released in the next few months, these changes will most likely only impact reporting years 2017 and beyond. Until then, my only advice would be to continue down your MU path as if nothing will change in 2016 and remain cautiously optimistic!
 Diana Strubler, Senior Product Analyst, Health IT Standards, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Senior Product Analyst, Health IT Standards, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.




Aaron Seret says
Thanks much Diana!
James Robertson says
I’m a nephrologist who’s not created templates in my “certified EHR” (EPIC) for dialysis facility rounding, because I couldn’t envision a scenario where the 3 “lesser” visits each month, if documented in Epic, wouldn’t burgeon those three “focus on one element of care” visits into the gigantic boilerplate-laden treatises that the MU program demands for routine office visits.
As you were, I was surprised to read of “the end of MU?”
There’s another wrinkle in this for me. What I’ve been using to document my dialysis rounding, until now, was whatever online tech was provided by the dialysis company (Falcon Dialysis at DaVita, Darwin at DCI, and SPIN MD at Satellite Healthcare clinics). Now I hear that MU will be repurposed; e..g, the tweets you post suggesting that we may be able to “customize” how we meet it. Do you have any sense of what that means for the shorter nephrology rounding visits most of us do because of the pre-HITECH, old-school mandate of “4 visits per month?” Will those visit notes (or do they now) require LOS, smoking status, allergies updates, patient visit summary notes, etc., to be considered part of making “meaningful use” of a “certified EHR?” Part of my reason for asking this now is that the dialysis company where I care for 90% of my ESRD patients (Satellite Healthcare) has just obtained “certified” status for its SPIN/SPIN MD software suite. I’m now even less clear on how and what I’ll be documenting at my dialysis patient visits than I am now, because I’ve been very happy using the “non-certified” products solely to help me take care of my patients, not to meet thresholds imposed by bureaucrats who never considered the dialysis clinic to be worthy of their attention.
Diana Strubler says
Hi Dr. Robertson,
The certification of SPIN could put you in an uncomfortable position to have to meet the current MU measures this year. Normally, Nephrologists have the luxury of taking the “50% rule” hardship exclusion because the systems at the dialysis facilities are normally not certified. Simply stated, the 50% rule is asking if more than half of your face-to-face encounters during the reporting period occur in a venue (or venues) equipped with a certified EHR. For those who do not meet this requirement – they can take a hardship exclusion from the MU program altogether. So take a look at all the non-hospital venues you see patients in – then tally a count of how many face-to-face encounters you have at a location with a certified EHR. If this amounts to more than 50%, you are stuck having to jump through the hoops of MU.
If you take a look at each of the NEW MU objectives – most need to be done during any of your non-hospital visits. Even during your basic dialysis rounds. However, the items that are bolded may not be applicable during each visit with your patient. Or you probably only need to do it once….
1. Perform a yearly HIPAA security risk analysis (not an encounter-specific measure, just something you need to do every year)
2. Have clinical decision support alerts turned on
3. Order meds, labs and rads using CPOE
4. e-prescribe
5. Securely send a patient’s summary of care to another provider (if they are transitioning out of your care) via secure email or some form of HIE
6. Hand out patient education materials (only to your office patients)
7. Perform med rec on all patients who came back into your care from another setting of care
8. Create portal accounts for your patients
9. Send patients secure messages (only need to do 1 of these this year)
10. Submit data to a public health agency or specialized registry (although there are some exclusions here that may apply to you)
So, as you look at your basic rounds in the dialysis unit, just keep the items above in mind. If you need to order labs/rads/meds – use your certified EHR to do so. Create portal accounts for your patients (this probably only needs to be done once – once they have access, then they have access). Hand out patient education materials to your office patients (if you have CKD clinics, identify some nice education materials to print out of your EHR).
The item I would focus on the most is #5 – that one seems to fall through the cracks quite a bit.
Who knows what the future of MU will hold… but one thing has been clear – this program has never favored Nephrologists!
I hope this helps!
Diana
To learn more about the 50% rule – read Dr. K’s fantastic post here: http://acumenmd.com/blog/unintended-consequences-nephrology-meaningful-use-and-the-50-rule/
To learn more about the NEW MU objectives for 2016 – take a look at CMS’ quick tips: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/2016_EPTableOfContents.pdf