In November 1962, Life Magazine published the Shana Alexander article, “They Decide Who Lives, Who Dies” about the dialysis selection committee in Seattle, Washington. This magazine story was written almost 2 ½ years after the Scribner Shunt provided chronic vascular access for Clyde Shields, making him the first chronic dialysis patient. Prior to Clyde Shields’ procedure in March 1960, End Stage Renal Disease was a universally fatal illness. Since 1960 dialysis has constantly evolved as a life-saving treatment through the efforts of patients, families, nephrologists, and other clinicians working to make it safer, better, affordable, and available to all who need it. In over 5 decades of chronic dialysis treatments, teams of social workers, dietitians, nurses, and patient care technicians have worked with patients and families to create a good patient experience for a difficult chronic therapy. Dialysis quality in all aspects is a matter of life and death.
Quality Dialysis Patient Care
Dialysis treatment quality has many facets. Respected organizations have exhaustively reviewed research data to create dialysis clinical quality guidelines for nephrologists, nephrology practices, and dialysis organizations. Electronic systems with data capture create the opportunity for routine reporting of standardized dialysis quality performance. Dialysis quality data is publically available in a variety of ways including on the Medicare.gov website Dialysis Facility Compare. Other non-profit organizations such as Arbor Research’s DialysisReports.org offer a clearinghouse of dialysis quality data with interpretation assistance for patients.
Patients or “consumers” making a decision about dialysis therapy choices should have access to meaningful data. The decision is complex and often truly life-saving. In addition to straightforward patient outcome data available to renal patients there are many excellent non-profit organizations such as the National Kidney Foundation (NKF), American Association of Kidney Patients (AAKP), and the Medical Education Institute (MEI), which offer education and information about making dialysis treatment choices.
It is clear that making a decision about quality dialysis care is complex, but having correct and credible data is essential.
Data Quality
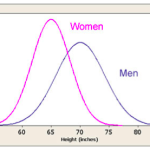
In recent blogs Terry has written about data concerns for the proposed dialysis center 5-Star rating system. “The Curse of the Bell Curve” post outlined the risk and confusion in applying a normalized Bell curve to non-normally distributed data. The proposed Bell curve distribution of the 7 variables in the 3 domains of “Ratios”, “Access”, and “Outcomes” are then simplified into the 5-Star rating of dialysis centers.
While the Bell curve treatment of the data is concerning, last week’s “Seeing Stars” post pointed out a more ominous feature of the 5-Star rating process; it is predicated on data that must be validated, complete, and credible. The integrity issues include missing data; Terry notes that 20% of dialysis facilities are missing data for at least one of the variables. Another data integrity point of concern is the heavy weight given to hypercalcemia when compared to Standardized Hospitalization Ratio (SHR) and Standardized Mortality Ration (SMR) as outcomes of greater significance to patient care.
Data Integrity
How important is data integrity?
Data integrity broadly defined refers to data accuracy and reliability. To be accurate the data must be complete; reliability is the assurance that the data is unchanged from the original true value over the data lifecycle. Certainly, data integrity characteristics include the processes to ensure health data security with safe and secure data transfer and storage.
Data Stewardship
In the current electronic health environment, data integrity also supports data stewardship: the oversight of health information collection, use, and disclosure. In a 2012 letter to then HHS Secretary, Kathleen Sebelius, the National Committee on Vital and Health Statistics (NCVHS) outlined the role of Data Stewardship in “using data to advance health.” NCVHS notes that data usage is complex and evolving due to the explosion of accessible clinical data making data stewardship crucial for leveraging data for the public good.
In an evolving definition the NCVHS links data integrity to data stewardship emphasizing that good data must be appropriately used:
- NCVHS 2009 definition of data stewardship: “…the responsibility of ensuring the appropriate use of information and included data collection, viewing, storage, aggregation, and analysis”
- NCVHS 2012 expanded data stewardship definition: “…includes the integrity of data because appropriate use presupposes that data are of reasonable quality to accurately measure what they are intended to measure.”
- NCVHS is by law the health information advisory body to the U.S. Department of Health. In a formal report to Congress on of the state of U.S. eHealth in 2012 and 2013, NCVHS notes that, “ …eHealth standards should be patient-centered and consumer-centered, resulting in better health care and better patient and population health at lower costs without compromising the quality or safety of care.” In the NCVHS vision for the future, “useful data and effective data stewardship” is a major theme in achieving this goal.
When considering dialysis treatment, patients deserve access to information to help them make choices. They deserve credible and meaningful data to make these choices. Our community, payers, and providers alike must commit to being good data stewards to ensure that the data we publish accurately represent the quality of care provided to patients. As NCVHS states in the conclusion of their report, “The principles of data stewardship are now well established; the work of translating them into practice will continue to evolve as the urgency of data stewardship grows ever greater in the future.” Urgent indeed.


Leave a Reply