 “Change is the law of life. And those who look only to the past or present are certain to miss the future.” —John F. Kennedy
“Change is the law of life. And those who look only to the past or present are certain to miss the future.” —John F. Kennedy
Do you like change? If you are a physician or work in a medical practice, I certainly hope you like change. Healthcare in general is changing and Health IT, in particular, is changing almost monthly. For example, while we’re scrambling to assimilate Meaningful Use (MU) Stage 2 requirements it’s time to get ready for Stage 3. Do you feel like Fred Flintstone peddling your feet as fast as you can go to keep your car on the road?
For the times they are a-changin’
Recently the Office of the National Coordinator for Health IT (ONCHIT) published its annual report to congress on Health IT (HIT) progress, which provides a preview of HIT in the next few years. This annual report meets ONC’s legal requirement to document planned actions to meet the goal of transforming U.S. healthcare to a digital healthcare system. The annual report provides an overview, but 2 other Health and Human Services (HHS) reports offer more detail: The Federal Health IT Strategic Plan and Connecting Health and Care for the Nation: A Shared Nationwide Interoperability Roadmap version 1.0. These reports describe “near-term health IT strategy” actions including:
- Ensuring electronic health information is appropriately available, easily transferable, and readily usable by the patient, provider, payer, scientist, and others
- Improving the safety and usability of HIT and allowing the market to function in a way to incent necessary improvements
- Simplifying program requirements to lower administrative burden and create a clear link between program participation and outcomes
The report also outlines expectations for the private sector as a commitment to:
- Help consumers easily and securely access their electronic health information
- Help providers share individuals’ health information with their patients and other providers whenever permitted by law, and not knowingly and unreasonably block electronic health information; and
- Implement federally recognized national interoperability standards, policies, guidance, and practices for electronic health information, and adopt best practices including those related to privacy and security
Changing rules and regulations along with CMS incentive and penalty programs will be levers to achieve a “secure, interoperable electronic health information infrastructure that seamlessly supports the health system and provides individuals with safe, person-centered care.”
Changes in meaningful use
The CMS Final Rule issued last October adjusted MU Stages 1 and 2 and established requirements for MU Stage 3. These CMS incentive programs will need to be reassessed this spring when the final rule for the Merit-based Incentive Payment System (MIPS) created by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) is published. After the October 2015 Final Rule publication, Stage 2 MU was changed to include:
- A reduction to 10 objectives, so that MU Stage 2 and Stage 3 are more aligned
- Removal of redundant or “topped out” objectives
- Fewer “patient action” requirements
- Leaving a 90-day reporting period for 2015
- Aligning to a single calendar-year reporting period for all providers
Diana Strubler and Terry Ketchersid provided MU Stage 2 details in previous Acumen blog posts.
New MU Stage 3 rules include:
- Continuation of the single calendar-year reporting
- Better alignment in reporting requirements among MU and other CMS quality reporting programs
- An attempt to include measure options that might be more meaningful for a provider’s practice
As Terry noted in his blog post from February 15, all of these quality programs are rudimentary and are in transition. In addition, after 2018 MU will be integrated into MIPS.
Changes in technology use
The ONC Annual Report includes a snapshot of the U.S. HIT environment in 2014. Adoption of EHRs started with the 2009 passage of the Health Information Technology for Economic and Clinical Health (HITECH) Act. Since then CMS HIT incentive programs like MU have significantly increased the use of technology in health care. Before 2009 40% of office-based physicians and 10% of hospitals were using some type of digital record. By 2014 74% of physicians and 97% of hospitals used a certified EHR.
In addition, other technologies such as smart phone applications have provided the opportunity for people to be more active in contributing personal health data. In 2014:
- 17% of people used a health-related smart phone app
- ~20% of people used text messaging to communicate with a health care provider
- ~33% of people emailed a health care provider
National survey results provided in the ONC annual report show how much change has occurred in the use of HIT, in part as a result of CMS incentive programs.
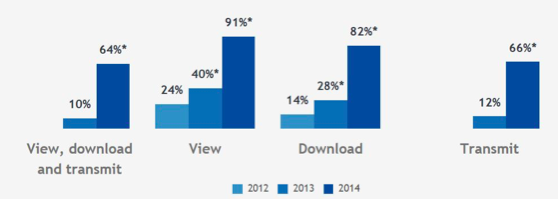
In 2014 hospital electonic systems provided many patient-centered activities. 91% of hospitals gave patients access to a medical record view and 82% gave patients the ability to download medical records. The change from 2012 is illustrated in this graph from the ONC annual report:
Figure 1: Percent of non-federal acute care hospitals that provide patients with the capability to electronically view, download, and transmit their health information
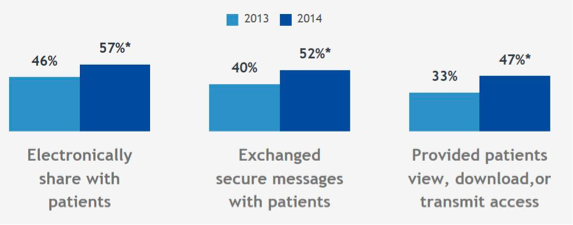
Physician offices have also made great strides in patient access to electronic records and in using technology to communicate with patients. In 2014, 47% of physicians gave patients medical record view, download, or transmit options. Here is the physician data from the ONC annual report:
Figure 2: Proportion of office-based physicians who electronically shared health information with patients in 2013 and 2014
Not enough change in interoperability
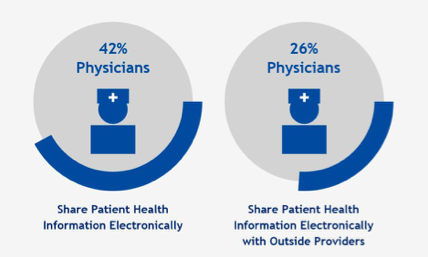
MU and other CMS programs have successfully incented HIT adoption, but a robust, fully functional HIT environment depends on true HIT interoperability. Hospitals have made some progress in sharing test results with external entities, but physician HIT interoperability is still poor. Here is the ONC annual report data:
Figure 3: Percentage of U.S. physicians sharing patient health data electronically as of 2014
ONC published Connecting Health and Care for the Nation: A Shared Nationwide Interoperability Roadmap version 1.0, which outlines HIT interoperability strategies. Interoperability is a key feature of the “learning health system in which health information flows seamlessly and is available to the right people, at the right place, at the right time.” With the achievement of widespread HIT adoption, the ONC and Health and Human Services (HHS) will now be focused on achieving greater interoperability. Interoperability incentive programs will be developed and may be part and parcel of value-based payment models like ACOs, which must have seamless data exchange among healthcare entities. Regulatory and business environments will change to standardize robust privacy and security and to prevent information blocking. There will be movement toward a shared or common set of technical standards like FHIR.
EHR adoption spurred by CMS incentive programs has changed the HIT landscape in just a few years. We can expect similar incentives will drive progress in HIT interoperability in the next 5 years as well. In the words of Bob Dylan:
“The line it is drawn
The curse it is cast
The slow one now
Will later be fast
As the present now
Will later be past
The order is
Rapidly fadin’
And the first one now
Will later be last
For the times they are a-changin’.”
 Dugan Maddux, MD, FACP, is the Vice President for CKD Initiatives for FMC-NA. Before her foray into the business side of medicine, Dr. Maddux spent 18 years practicing nephrology in Danville, Virginia. During this time, she and her husband, Dr. Frank Maddux, developed a nephrology-focused Electronic Health Record. She and Frank also developed Voice Expeditions, which features the Nephrology Oral History project, a collection of interviews of the early dialysis pioneers.
Dugan Maddux, MD, FACP, is the Vice President for CKD Initiatives for FMC-NA. Before her foray into the business side of medicine, Dr. Maddux spent 18 years practicing nephrology in Danville, Virginia. During this time, she and her husband, Dr. Frank Maddux, developed a nephrology-focused Electronic Health Record. She and Frank also developed Voice Expeditions, which features the Nephrology Oral History project, a collection of interviews of the early dialysis pioneers.




Leave a Reply