
I know it’s hard to believe, but the cold weather has arrived, and Thanksgiving is just around the corner. Before you know it, this decade will be in the rear-view mirror. Years from now, will the renal community remember 2019 as the year transformative payment models were hatched by CMMI? Or will we look back on a failed experiment? Hard to tell today, but one thing is certain, the Comprehensive Kidney Care Contracting (CKCC) models will be at the center of that discussion! The companion to Kidney Care First within the Kidney Care Choices model, CKCC is indeed the next version of the ESCO. CMMI has learned a few lessons from the ESCO experience and with stakeholder input they have crafted a series of total-cost-of-care models for Medicare beneficiaries with late-stage CKD and ESRD. We have learned some things about CKCC from the recently released RFA[ and through our conversations with CMMI, but many of the details are yet to be published. As you begin to plan for a big Thanksgiving celebration, let’s devote this post to unpacking this new 4-letter acronym.
3 options
The first thing you should know is CKCC comes in 3 flavors, largely distinguished by one’s appetite for risk:
- CKCC Graduated: Patterned in some respects after the SDO ESCO, there is an option for no downside risk in year 1. This option is intended for those electing to either exclude a dialysis provider or partner with a small dialysis organization, with fewer than 35 dialysis facilities.
- CKCC Professional: Participants share in 50% of the savings or losses for the total cost of care (Medicare Part A & B) for aligned beneficiaries.
- CKCC Global: Participants are at risk for 100% of the total cost of care (Medicare Part A & B) for aligned beneficiaries.
KCE
The new world is full of new acronyms and one you will come to know if you step up to the total-cost-of-care plate is KCE, or Kidney Contracting Entity. To play in the ESCO 2.0 sandbox, one must establish a KCE. Think of the KCE as the governing body for the CKCC models. All of the CKCC participants live here, and the KCE basically organizes the CKCC model and ensures everyone plays by the rules. The KCE must include nephrologists and it must include a transplant provider. Transplant provider is loosely defined such that it could be either a transplant nephrologist, a transplant surgeon, a transplant center, or an organ procurement organization. Dialysis providers are not required participants, but they will certainly be necessary in the Professional and Global models.
One last detail worth highlighting: the KCE must hold the financial guarantee. Just like we see in the ESCO program today, CMS will require the entity to demonstrate access to funds to cover losses in these total-cost-of-care models. The guarantee is calculated as 7.25% of the KCEs benchmark. To put that in perspective, the average benchmark in the 37 ESCO programs in 2017[ was just a hair under $74 million. I’ll let you do the math, but this is a lot of money and will require a partner with deep pockets.
Eligibility and alignment
Now that you have stood up a KCE, how do patients end up in your CKCC? Exactly like they do in the Kidney Care First model. CMS will look at claims data and align patients with your model based on outpatient encounters that nephrologist in the model have with eligible Medicare beneficiaries. For those with ESRD, they will look at the MCP claims. If your docs deliver 2 of 3 MCP visits over a 3-month period of time, the patient is in your model. If you stop doing so and the patient is no longer in market, CMMI will remove the patient from your model. For CKD? CMS will look for at least two encounters with a stage 4 or 5 patient during a 6-month period. They will identify the CKD stage based on the ICD-10 codes you put on a claim (N18.4 or N18.5). Any of the outpatient encounters listed in the table below must take place during the 6-month period.
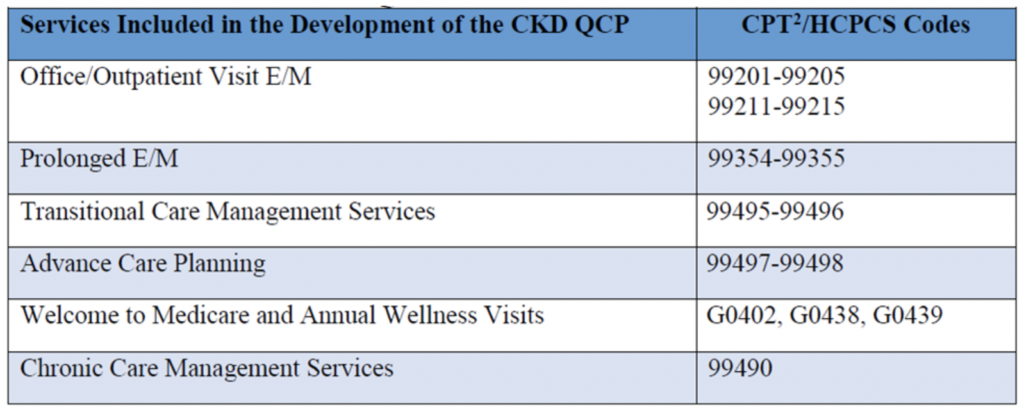
If an eligible late-stage CKD patient receives two or more of the services in the table above during a 6-month period of time, they are aligned to your model.
Size matters
I know we talked about patient counts last time with respect to KCF, but let’s revisit as I have some new intel here. The minimum patient counts for CKCC are 350 ESRD patients and 1,000 stage 4 or 5 patients. Acumen blog readers, I believe my back-of-the-napkin calculations may have been low in that recent KCF post. Try this at home: take a close look at the eligibility criteria and then examine how often you perform one of the services in the table above for Medicare primary patients. I think you will find you don’t see many late-stage Medicare primary CKD patients with that kind of frequency. So, I am throwing out that original napkin and now suspect that for KCF, the practices may need as many as 15 nephrologists to clear the 500 CKD patient count, and your KCE may need 30 or more nephrologists to meet the 1,000 CKD patient minimum. Fortunately, the KCE can aggregate practices, which may be required to meet the minimum patient count requirements.
Show me the money
I am sure I am wearing this phrase out, but it does tend to garner a lot of attention! So, how does a nephrologist get paid in CKCC? Well, in some ways you are paid like you would be paid in KCF, but there are some important differences, which I think could make CKCC more attractive than KCF. First you still receive the Adjusted MCP payment and the prospective CKD Quarterly Capitation Payment. The biggest difference in CKCC is those payments are not subject to the complex performance-based adjustment I described last time for KCF. (For those who missed this a few weeks ago, you can catch up by reading this post at your convenience.) You also collect that lucrative transplant bonus I described last time. The only difference is the bonus, which is worth up to $15,000 over three years and must be split up as follows: 20% to the nephrologists, 20% to the transplant provider, and the balance divvied up as the KCE sees fit.
But the real difference between KCF and CKCC is that CKCC is a total-cost-of-care model. Why is this important? Perhaps the best explanation is that the nephrologist has the opportunity to share in the savings generated when a hospital stay is avoided. Today, in a transactional fee for service environment, or within KCF in the future, all of that financial benefit accrues to the payer. But in a model where you are sharing in the savings created, you get to keep part (or in the Global model, all) of the savings you generate. Of course, there’s no such thing as a free lunch. And in CKCC, that opportunity to share in the savings comes with an equal opportunity to shoulder the loss, if losses occur. What you may ask, determines the financial target we are held accountable for in CKCC? The benchmark, of course.
Benchmarks
There are few things in a total-cost-of-care model that are more important than the methodology used to calculate the benchmark. One of the harshest criticisms levied against the ESCO program is the absence of transparency regarding how the ESCO benchmark is set. The RFA certainly does not contain the level of detail necessary to make a go/no-go decision, but from the modest perch of this blogger, they seem to be working towards a more transparent and predictable benchmark (emphasis on working towards). I will be the first to admit I am not an actuary, but at a very high level, here’s what seems to be happening:
The late-stage CKD patients and the ESRD patients in your model will each have a separate benchmark. Those benchmarks will be established by blending local claims’ historic experience with an adjustment to the Medicare Advantage book rate. CMMI plans to use U.S. Per Capita Cost to establish trend, removing yet another black box that exists in the ESCO program today. They plan to risk adjust the benchmark, but tell us in the RFA they will not use the HCC framework that’s widely used today, citing an effort to “mitigate the influence of coding intensity on risk adjustment.” We are unlikely to know the specifics about this new risk adjustment methodology until well after the RFA is due, but I would pay close attention to the approach they ultimately propose.
In addition to the benchmark components mentioned above, the Global CKCC model will face a 3% savings guarantee for the ESRD population, which will rise in future years. On a more positive note, if an aligned stage 4 or 5 patient remains in the CKD population for 12 months, the CKD benchmark increases by 1%.
Finally, the quality component of this set of Advanced APMs is enforced by what’s referred to as a quality withhold. Effectively, each CKCC model will see its benchmark drop by either 2.5% (Graduated) or 5% (Professional and Global). The CKCC has the opportunity to “earn back” the withhold based on performance on the CKCC quality measures below:
- Gains in Patient Activation (PAM) Scores at 12 Months; NQF #2483
- Depression Remission at 12 Months – Progress Towards Remission; NQF #1885
- Controlling High Blood Pressure; NQF #0018
- Optimal ESRD Starts; NQF #2594
Let me start by pointing out that 5% is a very big number. This is another area in which we will not have the detail we need to evaluate this feature until we see the participation agreement. But one might go so far as to say the attractiveness of these total-cost-of-care programs could depend on the intersection of the CKCC’s potential performance on these 4 quality measures and how that performance mitigates the withhold.
Advanced APM
Let’s not forget the impact participation decisions will have on your physician fee schedule. As all of you are aware, beginning in 2017, Medicare began paying physicians according to a new set of rules. The name of the new game is the CMS Quality Payment Program (QPP). The QPP creates two paths for providers: exposure to the Merit-based Incentive Payment System (MIPS) or participation in an Advanced Alternative Payment Model (APM), like the ESCO. Qualifying participants in an Advanced APM are excluded from MIPS and receive what amounts to a 5% bonus on their Part B book of business. When the ESCO comes to a close at the end of 2020, there remain two more years for these attractive Advanced APM features. As you consider these new models, it’s important to understand that the only one that is not an Advanced APM is the Level 1 option within Graduated CKCC.
Stuffing and gravy
So, what’s the upshot for the nephrologist? Well I hate to admit it, but it remains to be seen. At some point between now and the end of the year, we are likely to see a final rule related to the Mandatory ESRD Treatment Choices (ETC) model. Depending on how that unfolds, it could impact your decision regarding the pursuit of an application for one of the voluntary models. For those keeping score at home, the applications for these new voluntary models are due in 66 days. Of course, while the RFA sheds more light on the voluntary models, there is not enough detail in the RFA to weigh in one way or the other.
Importantly, you can apply for both KCF and CKCC. If both applications are accepted, you must pick one sometime before the end of next year, if you intend to play. CMMI has also made it clear there will be another round of applications in 2020 or 2021. But if you wait for the second solicitation, there is no free pass during the first year, as there is for this round of applicants. That is to say, if you wait, you will take downside risk out of the gate. Another point to consider, unless CMMI radically changes the alignment scheme for CKD, small- and even medium-sized nephrology practices will not be able to go it alone but will need to join other practices as permitted in order to meet the required minimum patient counts. With respect to CKCC, locating a transplant provider may become the bottleneck unless your practice includes a transplant nephrologist. And last but not least, while not required, I see no path to success in the Professional or Global CKCC options absent close collaboration with a dialysis provider.
At the end of the day, submitting an application is a risk-free endeavor. If your application is accepted by CMMI, a very close read of the participation agreement will certainly be in order before one decides to participate. Until we see that level of detail, we won’t know if we have a seat at the Thanksgiving table, or we are part of the meal. As always, the Acumen blog team will keep you posted as additional information emerges. In the meantime, all of us at the blog wish you a safe and sumptuous Thanksgiving!
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Photo by Element5 Digital on Unsplash



Leave a Reply