The Stage 2 MU objectives have received quite a bit of airtime since the final rule was published on August 23. One item that appears to be flying under the radar is the upcoming adjustment or penalty phase of the program. Buried near the end of the Stage 2 final rule are 30 pages that define the MU “payment adjustment.” The penalty does not begin until 2015; however, CMS will determine whom to penalize as early as next year. Let’s look at how the payment adjustment part of the program works.
The Adjustment
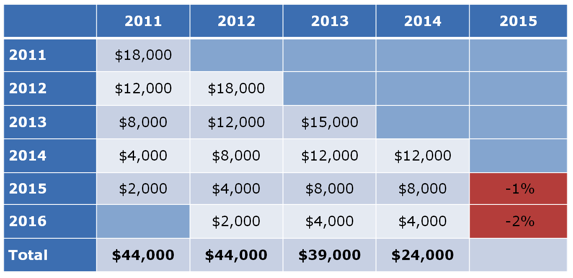
As you may recall, the incentive structure surrounding the Medicare component of the CMS EHR Incentive program consists of declining positive incentives which transition over time into financial penalties, also known as “adjustments.” The penalties are reductions in the providers’ Medicare Physician Fee Schedule (PFS) and they will begin in 2015 as noted in the 5th row in the table below.
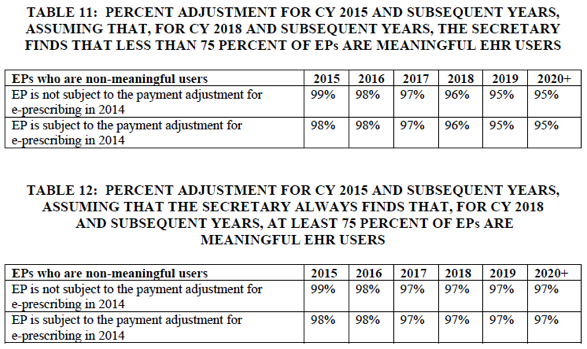
For example, if you are determined not to be a meaningful user for calendar year 2015, your Medicare PFS for 2015 will be adjusted by the applicable percentage, which in this case is 99%. The penalty increases by 1 percent per year until the adjustment reaches 97% in CY 2017. If the secretary of HHS finds that fewer than 75% of eligible professionals are meaningful EHR users, the penalty will continue its annual 100 basis point climb until the adjustment reaches 95% of the PFS in 2019. Tables 11 and 12 from the final rule define the penalties both in the circumstance where global utilization is less than 75% (table 11) and where it exceeds 75% (table 12). Note the last year of the eRx penalty supersedes the MU penalty in 2015.
Déjà vu
How does one avoid the penalty? The short answer is to demonstrate meaningful use. Of interest, CMS is determining who is a meaningful user very early in the game. The process is remarkably similar to the method employed by the CMS eRx program. Effectively, CMS will survey provider behavior well in advance of the year the penalty is incurred. The adjustment reporting period for the 2015 MU penalty is CY 2013 for the majority of nephrologists. If you demonstrated MU in either 2011 or 2012, CMS will determine if you did so in 2013. If you do not demonstrate MU in 2013, you will be on the list to penalize in 2015. For each year following 2015, the EHR reporting period for the payment adjustment is the calendar year two years prior to the payment adjustment period. There are a few exceptions to this rule noted below.
CMS points out the long lead time is necessary because “we sought to establish appropriate reporting periods for purposes of the payment adjustments in CY 2015 and subsequent years to avoid creating a situation in which it might be necessary either to recoup overpayments or make additional payments after a determination is made about whether the payment adjustment should apply. We noted that this consideration is especially important in the case of EPs because, unlike the case with eligible hospitals and CAHs, there is not an existing mechanism for reconciliation or settlement of final payments subsequent to a payment year, based on the final data for the payment year.” In other words, waiting to measure success in 2014 would be too late for the 2015 penalty.
Exceptions
Notwithstanding the above comments, CMS recognizes there are circumstances that fall outside the norm and as such they have created a set of exceptions to the rules reviewed above. Those exceptions include:
- Providers who never demonstrated MU prior to 2014. This group of providers must demonstrate MU during any continuous 90 days that ends at least 3 months prior to the end of 2014 in order to avoid the 2015 penalty. Eerily, that date coincides with the ICD-10 transition date (October 1, 2014).
- Providers who are new to the practice of medicine will receive a two-year exception from the payment adjustment.
- Providers who practice in multiple locations but do not control the availability of certified EHR technology in all locations.
- Extreme circumstances that exist outside the provider’s control (examples provided include your practice closing or a natural disaster destroying your EHR).
- Providers who have insufficient access to the internet.
- Providers who are non-hospital based anesthesiologists, radiologists or pathologists.
The first three on the list will have the greatest impact on nephrologists. In particular, keep your eye on the third exception on the list above.
Summary
Stage 2 of the meaningful use program will bring greater challenges to the practice of nephrology. By design, the measures are tougher and the thresholds are higher. EHR vendors will ensure their products are certified to meet these higher standards. As nephrologists prepare to meet the challenge, it will be important to fully understand the rapidly approaching adjustment phase of the program.

Lisa says
If we have filed for Meaningful Use Stage 1 for the past three years but decide not to file Meaningful use Stage 2 this year because the cost of implimention out weighs the incentive due in the fourth year of Meaningful use. Will be still receive a penalty for not meeting Meaningful Use for 5 years in a row.
Thanks,
Lisa
Terry Ketchersid, MD, MBA, VP, Clinical Health Information Management says
Hi Lisa,
The penalites are assessed on a year to year basis and do not consider what transpires in prior years. So yes, inspite of successfully attesting 3 years in a row, if you do not attest in 2015, you will receive the 3% penalty in 2017. If you do not attest in 2016, you will again be pnealized in 2018 (at least 3%). The exception would be if you can successfully file for one of the hardship excpetions. ONC tells us they will honor the hardship for 5 consecutive years (you have to file every year). In my view much will change over the next 5 years.
Rebecca Woods, Billing for Dr. Audrey Spencer says
We are in our 4th year of using MU. What is the penalty for not using it in our 5th year?
Terry Ketchersid, MD, MBA, VP, Clinical Health Information Management says
Hello Rebecca, the MU penalties are based on the calendar year, not on the number of years you participate in the program. Providers who do not participate in 2015 will face a 3.0% reduction in 2017 for all Medicare Part B charges. The penalty is the same for 4 year participants and for those who have never participated in the MU program.