 March is upon us, and with it comes the Madness that accompanies the end of the college basketball season. Although my preference would be to discuss BPI, RPI, and Kenpom today, something tells me you did not plan to spend a few minutes with the Acumen blog this morning to discuss college hoops. Instead, I will revisit a topic we have addressed in the past, but one that continues to create confusion. In my work with the Renal Physicians Association, I recently had the opportunity to unpack APMs. Today let’s explore them further.
March is upon us, and with it comes the Madness that accompanies the end of the college basketball season. Although my preference would be to discuss BPI, RPI, and Kenpom today, something tells me you did not plan to spend a few minutes with the Acumen blog this morning to discuss college hoops. Instead, I will revisit a topic we have addressed in the past, but one that continues to create confusion. In my work with the Renal Physicians Association, I recently had the opportunity to unpack APMs. Today let’s explore them further.
What’s an APM?
Alternative payment models, or APMs, represent new ways to pay for health care. Perhaps the best definition I have come across is the following: A system for medical reimbursement that provides additional compensation as an incentive for the delivery of higher quality and more cost-efficient health care by providers. I have highlighted a couple of important components in this definition. APMs pay providers an incentive above and beyond transactional fee for service, and that incentive is intended to drive better quality delivered in a more cost-efficient manner. APMs are part of the Medicare (and other payor) migration towards paying you for the financially efficient delivery of quality. Unlike transactional fee for service, where you are paid more if you do more, in these value-based programs you are paid more if you deliver “value” where value is loosely defined as:
Value = Quality / Cost
APM flavors
Medicare APMs are by and large operated by the Center for Medicare & Medicaid Innovation (CMMI). CMMI considers these models “experiments”, reflecting the fact that CMS is testing a variety of new payment models. From the perspective of nephrologists, APMs come in 3 flavors:
- Advanced APMs
- MIPS APMs
- Other APMs
Let’s consider each of these and the potential impact they have for nephrologists.
Advanced APMs
Advanced APMs represent the APMs CMS appears to be trying to attract docs to. That attraction is overtly based on a remarkable set of carrots. If you participate in one of these Advanced APMs, and the Advanced APM is determined to be a Qualifying Participant (QP), you avoid MIPS and collect a 5% bonus on your Part B book of business. The ESCO is the Advanced APM most familiar to nephrology. Last year every nephrologist in the 35 ESCOs with two-sided risk were determined to be QPs. The QP threshold remains the same in 2018. So, it would not surprise me if we see a repeat this year, with all participating nephrologists achieving QP status for 2018, avoiding MIPS in 2018 and collecting 5% of their 2019 Part B book of business as a lump sum payment in 2020.
What does it take to become an Advanced APM, you ask? CMS has established 3 criteria and each year the framework of every APM is bumped up against those criteria to determine if the APM is “Advanced”. Those 3 criteria are:
- Require participants to use CEHRT
- Base payment on quality measures comparable to those in MIPS
- Require participants to bear more than “nominal” financial risk
In my view, it’s the last criteria that largely separates Advanced APMs from MIPS APMs. Criteria 3 requires you to take downside risk. If the Advanced APM loses money, chances are you will write a check to Medicare (to share in the loss realized by the Advanced APM).
Every year, CMS publishes a list of the Advanced APMs. The list for 2018 includes:
- Bundled Payments for Care Improvement Advanced Model (BPCI Advanced)
- Comprehensive Care for Joint Replacement (CJR) Payment Model
- Comprehensive ESRD Care (CEC) Model (LDO arrangement)
- Comprehensive ESRD Care (CEC) Model (non-LDO two-sided risk)
- Comprehensive Primary Care Plus Model
- Medicare ACO Track 1+
- Medicare ACO Track 2
- Medicare ACO Track 3
- Next Gen ACO Model
- Oncology Model of Care (two-sided risk)
- Vermont Medicare ACO Initiative
Options 3 and 4 are the two-sided risk ESCOs.
MIPS APMs
The second category of interest to nephrologists is the MIPS APM. Three criteria also define a MIPS APM:
- Requires an agreement with CMS
- Includes at least one MIPS eligible clinician
- Bases incentive payments on performance in cost/utilization and quality measures
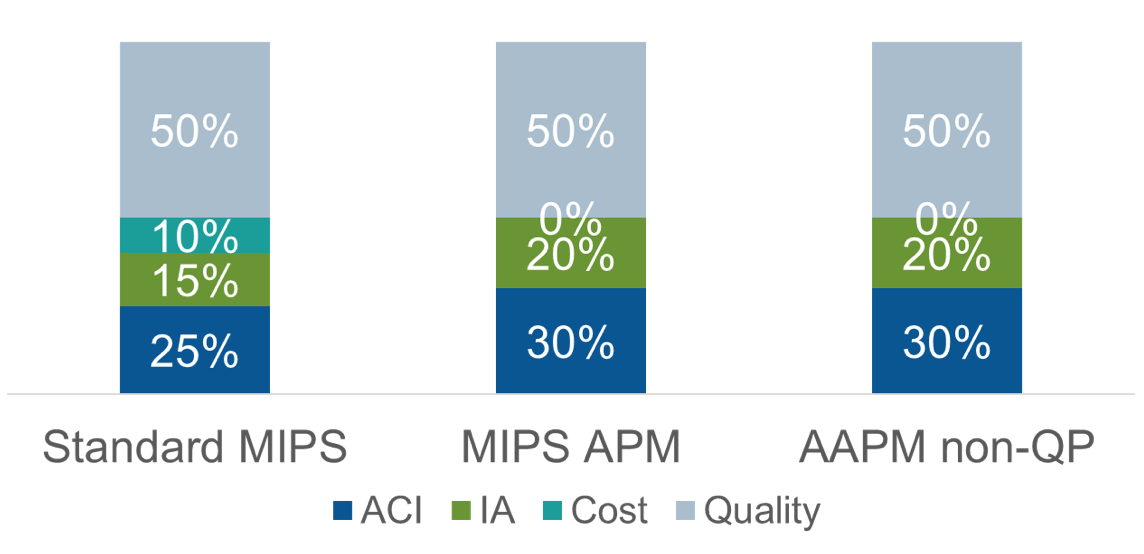
Perhaps the most common example of the MIPS APM is the Medicare Shared Savings Program (MSSP) track 1 Accountable Care Organization. This category of APMs is referred to as MIPS APMs because the docs participating in the APM must also participate in MIPS. There are 3 significant differences between participating in MIPS outside an APM and participating in MIPS within a MIPS APM. First, the MIPS categories have different weights. Notice in the figure below cost is not scored for the MIPS APM participants. The 10 MIPS points attributed to the Cost category in MIPS for 2018 is equally distributed to Advancing Care Information and Improvement Activities.
MIPS Category Weights
Second, the MIPS Quality and Improvement Activity categories are largely handled by the APM. The providers must pursue Advancing Care Information (ACI) as they would outside the APM, but with the APM picking up Quality and Improvement Activity, there is clearly less administrative overhead for the doc within the MIPS APM.
Finally, it’s important to understand every doc in the APM will receive the same MIPS score, and consequently the same Medicare fee schedule adjustment during the payment year. The ACI scores among the MIPS participants are basically rolled up into an APM-wide score and combined with the Quality and Improvement Activity scores. Bottom line, there is less overhead to report MIPS within an APM, but for better or worse, your performance very much depends on the performance of all of the other docs within the APM.
Other APMs
Last but not least we have the “other” category. These APMs largely do not require physician participation and as such are not eligible to receive the Advanced APM or MIPS APM designation. I mention them largely for completeness.
Is it Madness?
So where does all of this leave the typical nephrologist? As complicated as the Quality Payment Program is, I think CMS has tried to create an easier path for those willing to try out these new payment models. As part of my day job, I help a large team of folks shepherd a growing number of nephrology providers through the ESCO program. Last year all of the docs in the ESCO were exempt from MIPS in 2017 and will collect the 5% Advanced APM incentive in 2019. I have no doubt the same will occur this year. While that’s a good news story, all of those docs are taking downside risk and there’s no guarantee they will not have to write a check to CMS if the cost of care in their market exceeds the local ESCO financial benchmark.
Those of you participating in a MIPS APM will have an easier time participating in MIPS than will nephrologists exposed to MIPS outside of an APM. Your trade off? You don’t control your destiny. Your MIPS score (and therefore your fee schedule) depends of the performance of your fellow APM participants.
At the end of the day, one should recognize these models are being treated as experiments. Some will succeed; some will not. In my view it’s important for us to dip our toe in the water and get a taste for what the future may look like. At the Acumen blog, we will keep a close eye on things as they progress. Of course, we may join the rest of the country and take a few weekends off as the Madness of March begins.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Image from www.canstockphoto.com




Leave a Reply