
Greetings Acumen blog readers! I hope the dog days of summer are treating you well. It’s been a relatively quiet summer for nephrology, but after months of speculation, and with great fanfare, the administration recently unveiled the most sweeping changes our discipline has seen in decades. These changes have been put forth in support of 3 broad goals:
- Reduce the number of Americans developing ESRD by 25% by 2030
- 80% of new ESRD patients in 2025 will either start at home or start with a transplant
- Double the number of organs available for transplant by 2030
Piece of cake, right? Seriously though, while each of these goals seems aspirational, who among us would not get behind each of them with enthusiasm? As always, the devil is in the detail. The administration plans to use every tool in its arsenal to achieve these goals, many of which will become clearer over the next few months. Today let’s focus on the 5 (that’s right, 5!) new payment models announced 12 days ago that will impact how you are paid to care for patients with renal disease as early as next year.
Mandatory Model
Let’s start with a model that half of you may be exposed to beginning in a few short months. Coinciding with the Executive order issued on July 10, HHS released a 412-page proposed rule. Thankfully half of the rule is dedicated to a mandatory model for radiation oncology, but the other half is focused on patients with renal disease. The cleverly titled ESRD Treatment Choices (ETC) Model is a bold move to measure the impact physician- and dialysis-provider-facing financial incentives will have on both the home dialysis rate and the transplant rate.
At a high level, HHS plans to randomly divide the country in half, such that 50% of the country’s nephrologists and dialysis clinics are exposed to ETC and 50% are not. At the end of 6-and-a-half years they hope to have enough data to determine whether or not the incentives made a difference. The split across the country will be based on the Dartmouth Atlas Hospital Referral Regions (HRR). There are just over 300 HRRs around the country. CMS believes the HRR system provides the best opportunity to equally divide the country. Bottom line, if your practice’s ZIP Code is in one of the selected HRRs, you are in. If you are a JV partner and your clinic is in one of the selected HRRs, that clinic is in. According to HHS, we should know who’s in and who’s not before the end of this year.
ETC nuts and bolts
Basically, the ETC model will impact the MCP payments to nephrologists and the “72X” claims made to dialysis providers for those in the model. Each provider type (nephrologist and dialysis clinic) will face two incentives:
- Home dialysis payment adjustment (HDPA)
- Home dialysis and transplant performance assessment and performance payment adjustment (PPA)
HDPA is a declining bonus paid on top of home dialysis claims (MCP for the docs and 72X for the clinics). The proposed schedule looks like this:
- 3% bonus in 2020
- 2% bonus in 2021
- 1% bonus in 2022
When you do the math, the impact this will have on your bottom line is rather trivial unless you have a high home penetration today and/or you own a home dialysis clinic.
While HDPA is a bit of a sleeper, things get very interesting with the second adjuster, PPA. PPA is an asymmetric upside/downside adjustment to ALL MCP and 72X claims (home and in center). It’s set to begin with claims for dates of service after July 1, 2021, and will end with claims submitted on June 30, 2026. The excitement here is the dramatic range this incentive will take. For the nephrologist, out of the gate the maximum downside adjustment is a 6% penalty and the maximum upside is a 5% bonus. At the end of the program, the maximum penalty is 11% and the maximum bonus is 10%! That’s right, if this thing comes to fruition, in 6 years there may be docs receiving 89% of the prevailing MCP payment and there may be docs receiving 110% of the MCP. Even MIPS is not that dramatic (and the ranges for the dialysis clinic provider are even wider).
Modality Performance Score
How, you might ask, is the PPA adjustment determined? Well, by your modality performance score (MPS) of course. CMS intends to measure both the home dialysis rate and the transplant rate for every provider in the model. Your home rate will make up two-thirds of your score while your transplant rate will make up one-third. As with the ESCO quality scoring methodology, your rates will be compared with a benchmark, and your rates will be compared to your performance the prior year (i.e., you receive credit for achievement and for improvement, whichever is greater). Achieve a high MPS, and your MCP payment will be handsomely rewarded. Stick your head in the sand and continue business as usual, and your MCP payments from Medicare will take a substantial haircut.
NPRM
I mentioned the devil was in the detail, and I can assure you there’s far more detail in the NPRM[. Also, note this model is the only one which requires comment, and therefore it could change between now and the release of the final rule. However, in our experience, while some of the details may change, the final rule tends to look a lot like the NPRM. And speaking of detail, let’s conclude with a look at the 4 voluntary models, each of which are missing substantial detail.
Voluntary Models
In the same breath 12 days ago, 4 voluntary renal models were announced by CMMI. This announcement was essentially the “ESCO 2.0” many of us have been waiting for. The major disappointment in the eyes of this blogger? Unlike in the ESCO where the dialysis provider was a required participant, they are considered optional in the 3 total cost-of-care voluntary models. In spite of years of success in the somewhat flawed ESCO model, working collaboratively with nephrologists, dialysis providers were able to improve quality while lowering the total cost of care. Not requiring them as a participant in the new models seems a bit short sighted to yours truly, but I digress. Outside the limited information we have today regarding the voluntary models, the detail for these 4 models must await the arrival the of their respective Request for Applications (RFA) later this summer. But here’s what we know today. All 4 will reportedly share the following attributes:
- Timeline: They are expected to start Jan 1, 2020, and end Dec 31, 2023, with each having an option for 1 or 2 additional years.
- Alignment: Medicare patients are aligned to each
model in the same fashion. There are 3 types of patients that will be part of
these 4 models:
- Medicare beneficiaries with CKD stages 4 and 5
- Medicare beneficiaries with ESRD receiving maintenance dialysis
- Medicare beneficiaries who were aligned to a KCF practice or KCE by virtue of having CKD stage 4 or 5 or ESRD and receiving dialysis that then receive a kidney transplant
- Each model includes what sounds like a very lucrative bonus paid for each of the transplants accomplished during the model.
The 4 models have long names and of course a new set of acronyms for us to learn. They come in basically 2 flavors:
- Kidney Care First (KCF) Model
- Comprehensive Kidney Care Contracting (CKCC), which includes 3 versions
Kidney Care First
KCF is a nephrology practice-facing model which will be considered an Advanced APM. This is basically a professional fee capitation program in which nephrologists will be paid an adjusted capitated payment for each aligned patient for managing the care of late stage CKD (4 & 5) and ESRD patients. One way to think about this one is to imagine blending your MCP payments and the E&M payments you receive for taking care of late stage CKD patients. Instead of submitting claims with a CPT code (and making sure you capture the documentation necessary to justify said CPT code), you would receive an upfront PMPM to care for those patients aligned to you or your practice. We have been told in the recent past the new renal models will mirror the primary care model which CMMI announced a few months ago. Within Primary Care First, this professional fee capitated payment is adjusted up or down by quality performance and risk scores. Whether this happens within KCF remains to be seen.
Comprehensive Kidney Care Contracting
CKCC is quite a bit different than KCF. The first difference is that every CKCC that’s established must include a nephrology practice AND a transplant provider. Dialysis providers are optional. CKCCs are basically taking risk for the total cost of care for patients aligned to the model. CKCC comes in 3 flavors, each offering a different risk profile:
- CKCC Graduated Model: This model is based on the existing CEC Model One-Sided Risk Track, allowing certain participants to begin under a lower-reward, one-sided model and incrementally phase into greater risk and greater potential reward. This one resembles the small dialysis organization ESCO and when it’s upside only. It will not be considered an Advanced APM.
- CKCC Professional Model: This payment arrangement is based on the Professional Population-Based Payment option of the Direct Contracting Model, with an opportunity to earn 50% of shared savings or be liable for 50% of shared losses based on the total cost of care for Part A and B services.
- CKCC Global Model: This payment arrangement is based on the Global Population-Based Payment option of the Direct Contracting Model, with risk for 100% of the total cost of care for all Parts A and B services for aligned beneficiaries.
What’s next?
Again, I cannot emphasize enough how little detail we have today regarding the voluntary models, and of course the mandatory model is subject to a comment period, which will be followed by the final rule. Best we can tell, for the voluntary models we will see request for applications for each model in August or September. They will likely have a due date prior to the end of this year, and then in 2020 it’s off to the races. From the nephrologist perspective, I’d summarize these 5 models by comparing various aspects:
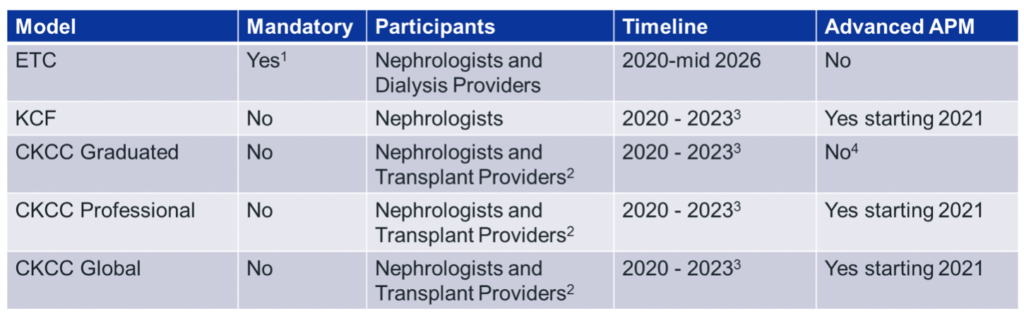
2Dialysis Providers and others are optional
3Option for 2 additional years
4CKCC Graduated can become an AAPM in later years
I call out the Advanced APM designation because after the ESCO concludes in 2020, the attractive Advanced APM incentives (avoiding MIPS and collecting a 5% bonus on your part B book of business) will be in play for two more years. There will be important physician fee schedule implications for these new voluntary models during performance years 2021 and 2022.
Navigating these new waters will be complex. Fortunately, Acumen blog readers have a trusted advisor at their side. Whether you are exposed to ETC, or considering one of the new voluntary models, Fresenius and Acumen stand ready to ensure your success. Over the past 4 years we have operated ESCOs from coast to coast that have made up well over 80% of the program, and together with our nephrology partners we have learned many important lessons about how to deliver better care to our patients in value-based care programs. Couple that with the value-based care resources available within Acumen 2.0, and we have a wonderful foundation to build on. We have more experience in this space than any other participant, and we look forward to working with each of you to advance renal care for all patients.
Do you have questions or comments about these new models? Drop us a comment and join the conversation.
Blog bonus section: New FLAs and TLAs
Frequently the announcement of new models arrives with a laundry list of new acronyms. I’ve used a few of them above and have pulled them together for your reference below.
CKCC: Comprehensive Kidney Care Contracting; 3 of the new voluntary models, which take risk on the total cost of care for ESRD and late-stage CKD patients and are set to begin January 1, 2020
ETC: ESRD Treatment Choices; the mandatory model reviewed in the proposed rule that will impact half of the nation’s nephrologists and dialysis providers beginning January 1, 2020
HDPA: Home Dialysis Payment Adjustment; a time-limited, upside-only bonus, which is part of the ETC model
HRR: Hospital Referral Region; A Dartmouth Atlas construct that will be used as the basis to randomly determine which half of the country will be involved with the ETC model
KCF: Kidney Care First; the voluntary model that places a nephrologist’s professional fees at risk
MPS: Modality Performance Score; a roll up of a provider’s home dialysis and transplant rates, which will determine the PPA adjustment within the ETC model
PPA: Home dialysis and transplant performance assessment and Performance Payment Adjustment; The upside/downside adjustment within the ETC model, which is determined based on the provider’s home dialysis and transplant rates
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Photo by John Bakator on Unsplash.




Dylan Steer says
Nice summary Terry. Thank you for taking the time to put together this informative and insightful blog post on a complex topic.
Navid Saigal says
Great article! Thanks Terry
CIndy Corpier says
Thank you, Terry for dispelling some of the fog. My impression is that nephrologists and dialysis providers will be on the hook for outcomes out of our control ie. doubling the number of transplants in 5 years, something that hasn’t occurred in twenty or more years. I’m also concerned that patients who are not transplant candidates or able to manage home therapies will be denied dialysis. Am I completely off base?
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Hi Cindy,
Great questions! My favorite response to these new models is the devil is in the detail. In the mandatory model we are paid based on home and transplant rates. But how they measure both are key. Looks like we will be compared with a benchmark rate that’s established in the half of the country that’s not in the mandatory model, AND compared with our own local year over year improvement. We will receive credit for both. Also they are establishing exclusions from the calculations (patients with dementia will not be in the home rate, the transplant rate has an age cut off)…a lot of additional detail. If there is an upside, its the fact that for the first 3 years we will face a small bonus for our home patients. But after that things truly get interesting. I think we will learn quite a bit more when the final rule is published later this year.
Chad Humphrey says
Thanks for the article Terry!
Amanda Williams says
I am assuming PD is included in reference to home dialysis?. We use the same CPT code for both home hemo and pd, so I am assuming this would apply to both.
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
That’s correct Amanda. They will be looking for 90965 and 90966 which will cover both PD and Home HD. Note the patients must be 18 years of age or older so only that age group within 90965 will be counted.
RG says
Do you anticipate some ESCO providers joining MIPS in 2021? Will that be a tough transition from an ESCO to a MIPS? When are the request for applications coming out? I was expecting them by now. How involved will the LDOs be in these new programs?
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Great question RG. Participating in MIPS in 2021 will depend on choices nephrologists make related to the new voluntary models. 3 of the 4 are intended to be Advanced APMs. Assuming one applies and is accepted to participate in one of the voluntary models, MIPS could be avoided in 2021 (and 2022) if the model was deemed a Qualifying Participant. CMMI tells us we will see the RFAs for the new models by the end of “summer”. I suspect we will have them in September. With the exception of KCF, I do not see how the new models succeed without the involvement of a dialysis provider, and even KCF will require some expertise which the average nephrology practice may not possess (actuarial analysis, an understanding of risk adjustment, etc.). I’d anticipate a follow up in the Acumen blog once we see the RFAs.
Dora says
Thank you very much for explaining each and everything. Nice Summary! Keep updating with such useful information!