Last week I had the pleasure of participating in the CMS kick-off call for the 2013 Registry season. This will be the fifth consecutive year our company has had the privilege of assisting nephrologists in reporting quality data to CMS. Leading this effort on behalf of CMS is Dr. Dan Green who combines a detailed understanding of the program with the good-natured perspective of a physician who has been in the trenches.
The evolution of quality reporting
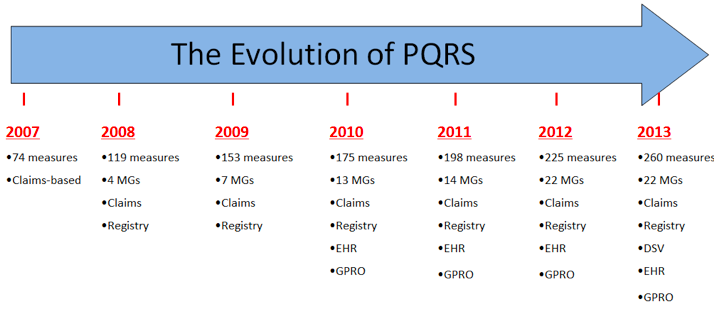
Looking back over the years it is remarkable how the PQRS program has expanded. Starting in 2007 with 74 individual measures, which required claims reporting, this year the program boasts 22 measures groups and 260 total measures. A glimpse at the graphic below should convince you that quality reporting is here to stay.
Today there are several ways to report PQRS, but Registry reporting remains widely popular among nephrologists because of its flexibility and ease of use.
Two important takeaways for 2013
As Dr. Green led us through the session last week, a couple of valuable lessons emerged from the National 2011 PQRS Registry experience. A couple of points are worth sharing in this forum:
- Make sure the Registry receives your correct TIN/NPI pair. When a Registry submits PQRS data to CMS on behalf of a provider, CMS uses the combination of the provider’s Tax ID Number (TIN) and the provider’s National Provider Identifier (NPI) to determine whom to pay. Note you should use your individual NPI and not the practice’s NPI. TIN/NPI mismatches remains one of the most common avoidable mistakes leading to no payment to the provider. In 2011 almost 75% of Registries submitting data to CMS submitted at least 1 TIN/NPI pair for which CMS could not find physician fee schedule charges. Stated another way, 5% of the TIN/NPI pairs submitted in 2011 fell into this bucket. The lesson is to make absolutely certain you provide the correct pair to your Registry in 2013 or you will receive 0.5 % of $ 0.00, which was nothing last time I checked.
- “Zero percent performance rates” don’t count. 2011 was the first year CMS added this nugget to the program. In effect this rule states that if an individual measure you are reporting has a performance rate of zero, CMS will treat this as though you did not report the measure. This applies to measures groups as well. If you report the CKD measures group, but one of the measures within that measures group has a goose egg for performance, you will not receive credit for reporting that measure. In other words, if the measure you are reporting has a zero in the performance numerator, CMS will not pay you an incentive. In my view, this is a very subtle step towards pay for performance. There are, however, “inverse measures” in which the quality actions are not counted in the measures numerator, and a zero percent performance rate is fantastic. For those measures, a 100 percent performance rate results in no payment. In our world, measure #123 (patients on ESAs-hemoglobin > 12), one of the four measures within the CKD measures group, is an inverse measure. One final point (which is explained in more detail below), your actions in 2013 will determine whether or not you are penalized in 2015. As such, reporting a measure with a zero percent performance rate will not get you paid in 2013, but it will count towards avoiding the 2015 penalty.
Will penalties drive utilization?
As Dan wrapped up the session, he made a couple of remarks related to the looming 2015 penalty. To date, PQRS participants have been “chasing” a financial incentive. In 2013, the incentive remains, although it drops to 0.5 percent of the provider’s Part B allowable. This year is also the payment-adjustment reporting period for 2015. As Dan pointed out last Tuesday, adjustment is a CMS euphemism for penalty. Bottom line, many participants in 2013 will not only be chasing the 2013 incentive, they will also be running away from the 2015 penalty. I suspect this change for 2013 will only sharpen demand for registry reporting. Participation in our PQRS Registry has significantly climbed year after year since we started in 2009. I suspect our experience this year will be no different.
Do you have questions about participating in PQRS in 2013? If so, drop us a comment and join the conversation.

rg says
Thanks for the wonderful post. I have a question. One doctor is leaving on Nov 22. Should we submit PQRS for him? We have a new doctor starting on Nov 1. Should we do PQRS for that doctor? Thanks in advance for your input. RG
Terry Ketchersid, MD, MBA, VP, Clinical Health Information Management says
Good questions RG,
For the doc who is leaving the practice I would consider submitting one of the measures groups via a registry for 20 patients if you beleive the resulting incentive would make it worthwhile from a finaicial perspective. If successful, next fall the practice or the doc will recieve 0.5% of this years Part B allowable.
The doc who is joining in Nov is a tougher issue. For that doc it is unlikely to be worth chasing the 2013 incentive, but you will want to avoid the 2015 penalty. For that doc I would pick an individual PQRS measure (perhaps one of the 4 contained in the CKD MG) and make sure that provider submits the appropriate QDC codes on the claims for a few encounters with eligible Medicare Part B patients. If the QDC codes make the trip to CMS for denominator eligible patient encounters, the doc will avoid the penalty. If that is too much of a hassle, you could spend the money to use a registry and submit just a few patients via the registry and the new doc would avoid the 2015 penalty.
RG says
We are just finishing up the reporting for 2013, and want to start thinking about 2014. Are the measures going to be the same? If so, we want to do some tweaking of our systems to see if we can make it go even more smoothly one year from now. If the PQRS measures are changing, what are they going to be? We did the CKD measures for 2013 (anemia, proteinuria, flu vaccine, bp). Thank!
Terry Ketchersid, MD, MBA, VP, Clinical Health Information Management says
2014 will look a lot like 2013 RG. Look for additional details in a future blog post-stay tuned!