 I recently had the opportunity to speak about value-based healthcare to a group of physicians and hospital administrators. Value based healthcare is a hot topic these days, and the temperature is rising in the aftermath of Secretary Burwell’s recent announcement regarding firm targets for Medicare spending related to value-based medicine. We’ve addressed value in this blog before and most would agree that value is fundamentally about the economically efficient delivery of quality. We frequently define it with a simple equation:
I recently had the opportunity to speak about value-based healthcare to a group of physicians and hospital administrators. Value based healthcare is a hot topic these days, and the temperature is rising in the aftermath of Secretary Burwell’s recent announcement regarding firm targets for Medicare spending related to value-based medicine. We’ve addressed value in this blog before and most would agree that value is fundamentally about the economically efficient delivery of quality. We frequently define it with a simple equation:
Value = Quality / Cost
As we’ve mentioned before, how one actually hangs a number on quality and cost is one of the greatest challenges facing value-based healthcare, but that challenge has not stopped the value-based healthcare train. One example of particular interest to nephrologists is the ESRD Seamless Care Organization (ESCO). The Center for Medicare & Medicaid Innovation (CMMI) is moving forward with the ESCOs and the planned start date of July 1 is right around the corner. As this ESRD-specific ACO model begins to take flight, we are beginning to see results from other ACOs which have focused on the general medical population.
ACOs
The phrase “accountable care organization” is tossed around a lot these days. Of interest to those of us in the nephrology space is the distinction between Pioneer ACOs and Medicare Shared Savings Program (MSSP) ACOs. The MSSP is a much larger program with participation that virtually blankets the country. To date there are over 400 Medicare ACOs around the country which touch about 1 in 6 of the nation’s Medicare beneficiaries. The MSSP is also a permanent program with plans on the table to expand into a “next generation” ACO as early as next year. Commercial payers are also jumping on this train as the number of insurer-sponsored ACOs continues to rise.
At a very high level, CMS attributes Medicare beneficiaries to an ACO by looking at primary care services rendered. If the plurality of those services are rendered by a member of the ACO, the beneficiary is attributed to the ACO. Importantly, CMS also calculates an expenditure benchmark. This is the projected Part A and B spend for the attributed beneficiaries, which CMS believes would occur over the course of the year if the ACO was not in place. At the end of the year, if quality targets are met, and the actual Part A and B spend is less than what was projected, the ACO has an opportunity to share in the “savings” it created for CMS. Of note, less than five percent of the MSSP ACOs are taking downside risk. For this minority of ACOs, if the actual Part A and B spend for the attributed population exceeds the projected benchmark, the ACO has the opportunity to write CMS a check, as they will share in the “loss” CMS incurred.
Pioneer ACOs
In contrast to the MSSP ACOs, you can think of the Pioneer ACOs as an early experiment. The Pioneer ACOs were launched in 2012 and specifically targeted large healthcare organizations experienced in the realm of managed care. Unlike the MSSP ACOs where downside risk is rare, the Pioneer ACOs required members to participate in both upside and downside risk. This makes the Pioneer experience particularly interesting to nephrologists contemplating ESCOs because the ESCO framework also requires two-sided risk out of the gate if the dialysis ESCO partner is a large dialysis organization. Within this context I read with interest an article published in JAMA this month which explored the impact Pioneer ACOs had for Medicare beneficiaries when compared with beneficiaries outside the ACO. CMS was delighted to report the cost of care for Pioneer ACO beneficiaries rose less than for non-ACO beneficiaries in the same market during the first 2 years of the “experiment”. Of note, the authors point out mean quality scores improved from 70.8% to 84.0%, and the mean quality score increased for 28 or the 33 individual measures.
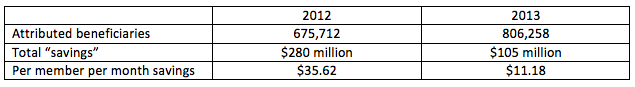
The financial benefit to CMS? I have summarized the overall financials from the paper in the table below. For the purpose of simplicity I am sharing the mean figures absent the confidence intervals:
Figure 1. Pioneer ACO Cost Reductions for CMS During Years 1 and 2
Lessons learned
What can we learn from this early experience? In the hands of experienced health care organizations which made up the original 32 Pioneer ACOs, costs declined when compared with non-ACO patients in the same markets. Notice the magnitude of the costs savings attained dropped significantly from year 1 to year 2, best demonstrated in the “per member per month” figure at the bottom of the table. Cost growth reductions spanned the health care continuum, but were most noticeable on the inpatient, or Part A spend side of the equation. In addition, when compared with non-ACO beneficiaries, the Pioneer patients had an increase in the frequency with which they were seen within seven days of hospital discharge.
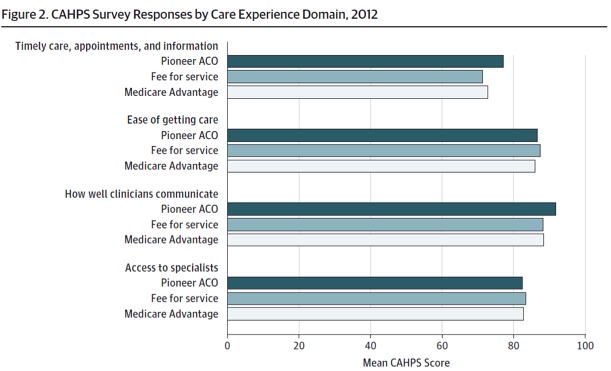
It’s important to note many of these ACOs are in markets like Boston where the penetration of commercial risk contracts is high, or in California where providers are well versed in the concepts of managed care. Finally, the paper spent a bit of time highlighting the patient experience of care as measured by a variety of CAHPS survey results. For those of you who do not believe patient satisfaction is an important part of the value equation, I call your attention to figure 2 from the JAMA paper which I’ve inserted below:
Last but not least, I should mention there has been a bit of attrition with the Pioneer program. Initially scheduled to run for three years, the Pioneer program has seen 14 of the original 32 ACOs withdraw from the experiment—many doing so because they were losing money.
ESCOs
I think the lessons above are valuable for the nephrology community to consider as we start down the ESCO path. There are clear differences between the two models (higher spend, fewer patients, and fewer participant providers in the ESCOs for example), but we should take note of the early experience of these Pioneers. While some have died with arrows in their backs, the majority have prospered and forged a new path, proving quality can be maintained or improved while costs are reduced. What are your thoughts about ACOs and ESCOs? Drop us a note and join the conversation.
 Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.
Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.




Leave a Reply