 It’s the week of Thanksgiving, my favorite holiday of the year. It’s the week where I imagine channeling my inner Martha Stewart and cooking up a feast that will have everyone talking. However, the reality usually hits the day before, when I realize I did not prepare enough and I have to cut corners (like the store-bought pumpkin pie). Will the store-bought pumpkin pie have the same quality as a homemade one? Nope, probably not, but it was easy and got the job done. The choice of going the down the easy path vs doing extra work for a better result is a theme I expect providers to face in 2015 with PQRS.
It’s the week of Thanksgiving, my favorite holiday of the year. It’s the week where I imagine channeling my inner Martha Stewart and cooking up a feast that will have everyone talking. However, the reality usually hits the day before, when I realize I did not prepare enough and I have to cut corners (like the store-bought pumpkin pie). Will the store-bought pumpkin pie have the same quality as a homemade one? Nope, probably not, but it was easy and got the job done. The choice of going the down the easy path vs doing extra work for a better result is a theme I expect providers to face in 2015 with PQRS.
The 2015 Medicare Physician Fee Schedule final rule (released on Halloween) ramped up the requirements for PQRS reporting. The 1,185-page document contained several notable changes:
- No carrot this year.Unsuccessful participation in PQRS results in a 2% reduction in your Medicare Part B allowable charges.
- Additional penalty. Unsuccessful or poor participation can also result in an additional reduction via the value-based payment modifier.
- Same options, fewer measures. All PQRS reporting options that were available in 2014 are also available in 2015, although the list of claims-based measures got quite a bit smaller.
- Measures lost and gained. CMS removed a total of 50 measures and added 20.
- Changing what success looks like. PQRS success means submitting 9 individual measures across 3 national quality strategy domains (including one cross-cutting measure). This doesn’t apply if you take the PQRS registry measures group route…more on this in a bit.
Although there are many ways to report PQRS as a nephrologist (i.e., claims, qualified registry, direct EHR, EHR data submission vendor, the Group Practice Reporting Option (GPRO) web interface, and the QCDR), I’d like to highlight the 2 options I believe will be popular this year: qualified registry and direct EHR reporting.
Qualified Registry Reporting
Providers planning to report via a qualified registry will notice that this option got quite the face lift in 2015. Providers still have the option of reporting either individual measures or a measures group, but the process for each got slightly more difficult.
The individual measures route now requires reporting on 9 measures, covering at least 3 of the NQS domains for at least 50% of the eligible professional’s Medicare Part B FFS patients seen during the reporting period. In addition, if the provider sees at least one Medicare Part B patient during the reporting period, he/she will need to ensure that one of the 9 measures is a cross-cutting measure. In the past, providers only had to report on 3 individual measures.
The other qualified registry route is reporting a measures group. CMS is maintaining the option to report via a measures group for at least 20 patients (11 being Medicare Part B patients). This option has been very popular for nephrologists in the past because of its CKD measures group offering. However, the 2015 final rule changed the definition of a measures group to now consist of at least 6 measures. In addition, CMS will retire one CKD measure (PQRS #123: Patients on ESA – Hemoglobin Level > 12.0 g/dL) while adding 3 new measures.
The 3 measures being added are highlighted in green below. More information about these measures will be available later this year.
Chronic Kidney Disease (CKD) Measures Group for 2015 and Beyond
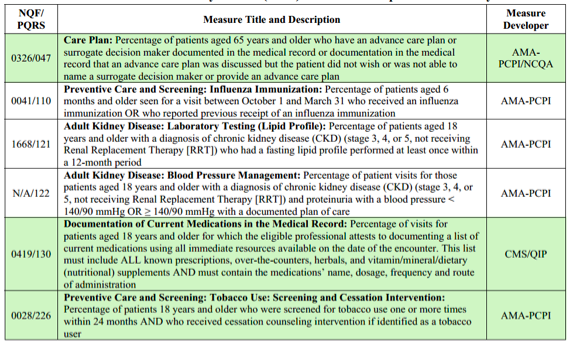
Source: 2015 Medicare Physician Fee Schedule Final Rule, Table 60.
Direct EHR Reporting
The direct EHR reporting option allows a provider to take the “two birds with one stone” approach when it comes to reporting CQMs for both PQRS and Meaningful Use. The rules for both programs are the same – report 9 measures across 3 NQS domains. Once your reporting period is finished, your EHR vendor (if able to) will ship your data off to CMS. This option may sound like a no-brainer for those participating in meaningful use, but there are still some points to consider:
- There are no CKD or ESRD measures offered for EHR reporting. There may be some generic measures that you can choose from to make up your total set of 9, but will your performance scores take a hit? Remember, this is the first year where groups under 100 will be subject to the value-based payment modifier.
- The population of patients being reported is a lot higher. Providers will report on all patients seen for eligible encounters during the entire 12-month period. This can be an issue when you are near the end of the year and notice your performance scores are low – recovering will be more of a challenge.
- Will you be in a full-year reporting period in 2015? HIMSS, MGMA, AMA and 14 other healthcare organizations sent a letter to the HHS Secretary calling for immediate action to amend the 2015 meaningful use reporting period and repeat another 90-day reporting period. If this comes to pass, the MU and PQRS reporting periods will once again be out of alignment.
- Are you taking a hardship exemption for Meaningful Use in 2015? Reporting via Direct EHR reporting may be too burdensome for providers who are opting out of MU in 2015. I would suggest looking at other options (such as a qualified registry or a QCDR).
What should you do?
Out of the two reporting options listed above, the qualified registry seems like it will be a popular choice again in 2015. It may not be as easy as reporting via a direct EHR (assuming you are also reporting MU for a full year), but qualified registry reporting provides more renal-friendly measures, which will most likely allow you to obtain a better performance score. Also, if you choose to report on a measures group, you only need to report on 20 patients.
There are other options for PQRS reporting that you can consider besides the ones I highlighted. If you have had success with claims-based reporting in the past then you may want to continue down that road (making sure the measures you reported in the past haven’t been retired). You may also want to consider the recently added Qualified Clinical Data Registry (QCDR) reporting option. This would allow you to use renal-specific measures, but it probably won’t check the box for reporting Meaningful Use CQMs.
It’s no wonder that 70% of the 48,000 physicians surveyed by MGMA rated Medicare’s quality reporting requirements as “very” or “extremely” complex. There are a plethora of choices – all of which have their own pros and cons. So start exploring your options early!
 New to the Acumen Blog is Diana Strubler, Senior Product Analyst, Health IT Standards. Diana joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS. We look forward to sharing more posts from Diana in the months to come!
New to the Acumen Blog is Diana Strubler, Senior Product Analyst, Health IT Standards. Diana joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS. We look forward to sharing more posts from Diana in the months to come!




Rg says
It was great catching up with the Acumen folks at the ASN meeting. Do you know if the PQRS scores are going to be posted on a public website? Also, for the VBM, did you mean greater than 100 providers (not less than)? Thanks for providing the nephrology community with these important regulatory updates.
Diana Strubler, Senior Product Analyst, Health IT Standards, Acumen Physician Solutions says
Hi Randy,
Thanks for being my first blog commenter (and an early morning one to boot)! The PQRS scores will not be posted publically yet…CMS is planning a phased approach for the physician’s compare website. The only thing that will be displayed publically in 2016 is if the provider successfully participated in the program in 2015.
As for the VBM…it can be quite confusing and Dr. K will be reviewing this information in next week’s post. 2015 is the performance year for the 2017 VM adjustment and during 2015 practices of all sizes will be under review. Practices with 9 or fewer providers will be “held harmless” with respect to the VM in 2017 (no downside risk), but they must successfully report PQRS in 2015. If they do not, they will face a 2.0% VM penalty in addition to the 2.0% PQRS penalty.