Last month, I had us humming the Sam Cooke classic “A change is gonna come” after CMS released a statement that modifications to Meaningful Use in 2015-2017 were on their way. Well, the changes are finally here (the proposed changes anyway).
On April 10, CMS released a 210-page proposed rule, with hopes to “better align reporting periods for providers, support a flexible, clear framework to reduce provider burden, and ensure future sustainability of the Medicare and Medicaid EHR Incentive Programs.” The proposed rule was CMS’ interim response to stakeholder concerns about the program’s complexity and hard-to-achieve reporting periods before Stage 3 changes take effect.
Overall, the proposed rule suggests:
- An overall simplification of the program aligned to the overarching goals of sustainability as discussed in the Stage 3 proposed rule
- Changing the reporting period in 2015 (for everyone) and 2016 (for new participants)
- Changing thresholds to patient engagement measures
- Reducing the number of meaningful use objectives to improve advanced use of EHRs
- Removing redundant measures and those that have become widely adopted (aka “topped out”)
Back to 90 days in 2015
One of the assumed changes announced in the proposal includes moving the 2015 reporting period to a continuous 90-day period within the calendar year. With enormous pressure from Congress, industry stakeholders and physicians, CMS backed away from the original calendar-year reporting period with hopes that the shortened reporting period in 2015 would allow providers more time to understand the provisions of the 2015-2017 rule.
Therefore, in 2015 all providers (regardless of their prior participation in the program) can attest to a continuous 90-day period within the calendar year. In 2016, all providers (except for new participants in the program) will have to go back to full calendar-year reporting. In 2017, all providers (regardless of prior participation) will be required to report the full calendar year.
A Single Set of Objectives Regardless of Stage
The proposed rule suggests that starting in 2015, all providers (regardless of what stage they are currently in) must attest to certain objectives and measures found in Stage 2. If a provider is scheduled to be in Stage 1, he/she will participate in a modified version of Stage 2 that will allow him/her to have special exclusions to the measures found only in Stage 2 and not in Stage 1.
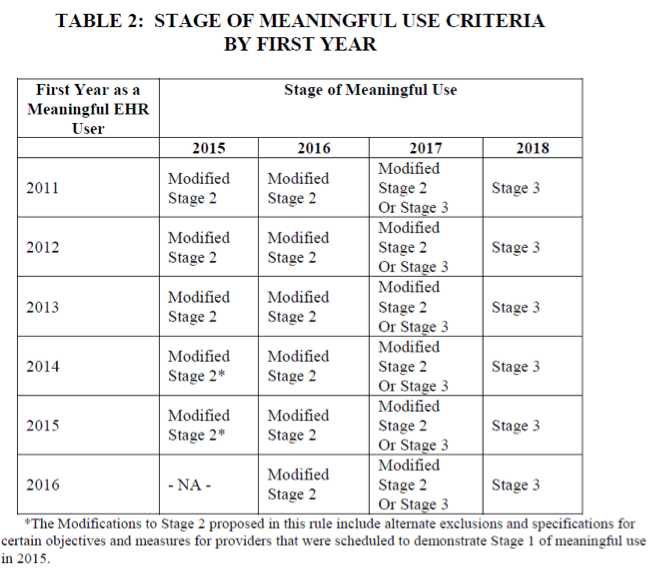
The stage progression can be found in the table below:
Measures Sent into Retirement
In order to simplify Stage 1 and Stage 2, CMS identified measures to remove from the program because they are “redundant,” “duplicative,” or “topped out.”
The following EP measures to be removed are:
- Record Demographics
- Record Vital Signs
- Record Smoking Status
- Clinical Summaries
- Structured Lab Results
- Patient List
- Patient Reminders
- Summary of Care
- Measure 1 – Any Method
- Measure 3 – Test
- Electronic Notes
- Imaging Results
- Family Health History
CMS makes it clear that removing these measures from the meaningful use program should not suggest that these are no longer best practices or discourage providers from conducting and tracking these activities for their own quality improvement goal.
Changes to Existing Measures
CMS not only removed a large list of objectives, it also made proposed changes to a few existing measures (specifically to the patient engagement measures that require patient action).
The proposed changes are as follows:
- Changing the threshold from the Stage 2 Objective for Patient Electronic Access measure number 2 from “5 percent” to “equal to or greater than 1.” In other words, only one patient must view, download, or transmit his/her health information.
- Changing the threshold from the Stage 2 Objective Secure Electronic Messaging from a percentage-based measure to a yes-no measure stating the “functionality fully enabled.”
- Consolidating all public health reporting objectives into one objective with measure options following the structure of the Stage 3 Public Health Reporting Objective.
Farewell Menu Set
Stage 1 and Stage 2 have always offered both core objectives and menu objectives. However, in order to simplify the program, CMS decided to eliminate all menu objectives and offer a shorter list of “core” objectives instead. For providers scheduled to be in Stage 1, this means that three current menu objectives would now be required:
- Perform Medication Reconciliation
- Patient Specific Educational Resources
- Public Health Reporting Objectives (multiple options)
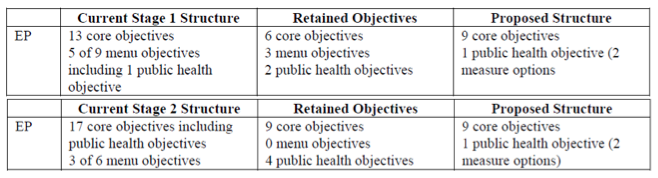
With the removal of measures and consolidation of Stage 1 and Stage 2, all providers in 2015-2017 will be required to successfully meet a total of 9 objectives plus 1 public health reporting objective.
NOTE: Stage 1 providers can use new exclusions for measures only found in Stage 2.
The Proposed 9 Core Objectives and Public Health Measure Options
- Protect Electronic Health Information
- Measure: Perform a security risk analysis.
- Clinical Decision Support
- Measure 1: Implement five clinical decision support interventions related to four or more clinical quality measures at a relevant point in patient care for the entire EHR reporting period.
- Measure 2: The EP has enabled and implemented the functionality for drug-drug and drug allergy interaction checks for the entire EHR reporting period.
- Computerized Provider Order Entry (CPOE)
- Measure 1: More than 60 percent of medication orders created by the EP during the EHR reporting period are recorded using CPOE.
- Measure 2: More than 30 percent of laboratory orders created by the EP during the EHR reporting period are recorded using CPOE.
- Measure 3: More than 30 percent of radiology orders created by the EP during the EHR reporting period are recorded using CPOE.
- E-Prescribing (eRx)
- Measure 1: More than 50 percent of all permissible prescriptions, or all prescriptions, written by the EP are queried for a drug formulary and transmitted electronically using Certified EHR Technology.
- Summary of Care:
- Measure 1: The EP that transitions or refers their patient to another setting of care or provider of care that (1) uses CEHRT to create a summary of care record, and (2) electronically transmits such summary to a receiving provider for more than 10 percent of transitions of care and referrals.
- Patient Education
- Measure 1: Patient-specific education resources identified by Certified EHR Technology are provided to patients for more than 10 percent of all unique patients with office visits seen by the EP during the EHR reporting period.
- Medication Reconciliation
- Measure 1: The EP performs medication reconciliation for more than 50 percent of transitions of care in which the patient is transitioned into the care of the EP.
- Patient Electronic Access
- Measure 1: More than 50 percent of all unique patients seen by the EP during the EHR reporting period are provided timely (within 4 business days after the information is available to the EP) online access to their health information.
- Measure 2: At least one patient seen by the EP during the EHR reporting period (or their authorized representatives) views, downloads, or transmits his or her health information to a third party.
- Secure Electronic Messaging
- Measure 1: During the EHR reporting period, the capability for patients to send and receive a secure electronic message with the provider was fully enabled.
In addition to reporting the objectives above, EPs must also report on either 1 or 2 public health reporting measures. Providers scheduled to be in Stage 1 must choose 1 of the possible 5 measures. Providers scheduled for Stage 2 must choose 2 of the possible 5 measures.
- Immunization Registry Reporting
- Syndromic Surveillance Reporting
- Case Reporting
- Public Health Registry Reporting
- Clinical Data Registry Reporting
NOTE: A measure from options 1-4 must be selected.
Ready…Set…Hold On…
All the changes noted above are not set in stone. A 60-day comment period is now underway. Once CMS filters through the comments, they will make any necessary changes and release a final, hopefully by the end of Summer. Although it’s safe to assume that everything proposed will probably stick (or even get easier), I would still proceed with caution until a final announcement is made.
Do you think CMS hit the mark with the proposed changes? Are the changes to the reporting period and objectives more attainable or is there still more work to be done? Sound off below!
 Diana Strubler, Senior Product Analyst, Health IT Standards, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Senior Product Analyst, Health IT Standards, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.



Andrew says
Nice summary!