 2014 is well underway and many nephrology practices are determining which reporting period to select as they contemplate participating in the meaningful use (MU) program this year. If 2014 is not your first year to participate in this program, you have the opportunity to pick the calendar quarter that will define your 2014 reporting period. As you may recall, the ICD-10 transition date is scheduled to occur on October 1, 2014. Because of this, I would suggest doing everything possible to avoid selecting the fourth quarter as your 2014 MU reporting period.
2014 is well underway and many nephrology practices are determining which reporting period to select as they contemplate participating in the meaningful use (MU) program this year. If 2014 is not your first year to participate in this program, you have the opportunity to pick the calendar quarter that will define your 2014 reporting period. As you may recall, the ICD-10 transition date is scheduled to occur on October 1, 2014. Because of this, I would suggest doing everything possible to avoid selecting the fourth quarter as your 2014 MU reporting period.
The 50% Rule
Beyond cautioning against Q4, I want to dedicate this post to a topic I continue to receive questions about. Those of you who understand our old friend the “50% Rule” like the back of your hand can tune in next week, but for everyone else, let’s take a deeper dive and sort out some of the confusion that persists.
The 50% rule establishes one’s eligibility to participate in the meaningful use program. In order to participate, at least half of the provider’s outpatient encounters during the reporting period must occur in a location or locations equipped with certified EHR technology (CEHRT). With respect to nephrology, the phrase “outpatient encounter” refers to every patient encounter you have during the reporting period other than those for which you used “place of service” code 21 (inpatient, hospital) or 23 (emergency room, hospital) on the claim you submitted to a payer. Telemedicine encounters are also to be counted, but in my experience few nephrologists have dipped their toe into the telemedicine ocean to date.
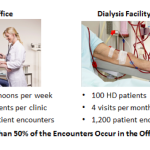
Let’s take a closer look at the impact of the 50% rule by examining three different scenarios.
1. Most outpatient encounters occur in the office
In this scenario, during the calendar quarter I elect to report meaningful use in 2014, let’s assume:
- I have 800 patient encounters in the office where I am using CEHRT,
- I have 600 patient encounters in a dialysis facility, and
- The dialysis information system deployed in the dialysis facility is not certified for meaningful use.
The vast majority of dialysis information systems are not certified for meaningful use, in large part because dialysis facilities (like nursing homes and ambulatory surgery centers) are excluded from participating in the meaningful use program. That is to say, in contrast to the hospital setting, CMS does not recognize these venues of care as eligible providers with respect to the meaningful use program.
This example in this first scenario is pretty straightforward. When the provider submits his or her 2014 meaningful use attestation, that attestation would only include the MU-related information that was collected during the calendar quarter for those 800 office-based encounters. Because the 600 dialysis encounters occurred in an environment not equipped with CEHRT their inclusion would be optional. Most would not include the dialysis patients here as their inclusion requires duplicate data entry (once in the dialysis information system and once again in the office-based CEHRT).
There are two caveats to mention here:
- If this provider does not participate in meaningful use in 2014, he or she will incur a 2% penalty in 2016, unless a hardship exception is successfully submitted prior to July 1, 2015.
- The provider may, at his or her discretion, access a certified EHR from within the dialysis facility and record patient data for those 600 dialysis patient encounters and still not include them in the 2014 meaningful use attestation. For example, the provider might decide he or she prefers to capture the MCP note in his or her certified EHR, or keep track of information related to billing in the CEHRT. In doing so, the provider is not compelled to report meaningful use objectives for this group of encounters.
2. Most outpatient encounters occur in the dialysis facility
This is the perhaps the most common scenario, in large part because many in-center dialysis patients are seen weekly. In this scenario, let’s assume:
- I also have 800 patient encounters in the office where I am using a certified EHR, but
- I have 1,200 encounters in the dialysis venue of care, and
- The dialysis information system is not certified.
In this situation, I have a choice to make, a choice made very clear by Travis Broome of CMS during last year’s National Provider Call (look specifically at the Q & A beginning at the top of page 30 of this transcript). In this case the provider has three choices for 2014:
- Do not report meaningful use and incur the 2% penalty in 2016.
- Do not report meaningful use and successfully file for the hardship exception that states more than half of your outpatient encounters occurred in a location(s) not equipped with CEHRT, AND the decision to deploy CEHRT in those venues of care was outside of your direct control. Note: If you are an independent owner/operator of a dialysis facility this hardship exception is not for you. Also note the hardship exception form posted on the CMS website today is only to be used to document what you did last year in order to avoid the 2015 penalty. Do not use this form for the 2014 reporting period.
- Access your office-based certified EHR from within the dialysis facility and duplicate the data entry (once in the dialysis information system and once in your office-based EHR) necessary to meet the meaningful use objectives for those patients encountered in the dialysis facility.
3. Most of the practice’s outpatient encounters occur in a dialysis facility, but mid-level providers see many of these patients
This is a common scenario in larger practices. Suppose the following:
- I have 800 patient encounters in the office, and
- There are also 1,200 encounters in the dialysis facility, but I make half of those dialysis visits and my nurse practioner or physician’s assistant makes the other half.
From a meaningful use perspective, the math has now changed as I have 800 encounters in the office and 600 face-to-face encounters in the dialysis facility during the meaningful use reporting period. My options in this scenario are identical to the choices the provider faced in the first scenario and the caveats identified in that scenario apply here as well.
Do the math
The three scenarios we walked through cover most of the circumstances I have encountered in nephrology practices around the country. But let’s face it, there are a number of permutations and combinations out there, particularly for those of you seeing patients in an access center. It’s important to do the math for your particular circumstance in order to better understand where you land with the 50% rule. If your specific situation is not covered above or if you still have questions about the 50% rule, drop us a comment below and we will help sort it out.
Certify the DIS?
Some have scratched the surface of the 50% Rule’s impact upon nephrology and have naively suggested the solution to this unintended consequence is to take the dialysis information system through one of the meaningful use certification paths. I heard this view most recently expressed a few weeks ago when I had the privilege of joining other stakeholders from the renal community as we met in Washington, DC, with representatives from ONC and CMS.
I have taken a very close look at the prospect of certifying the dialysis information systems and believe this is actually one of the worst things we could do. If patient care were clearly better in an environment where care delivery was facilitated by a certified EHR as opposed to an environment where the EHR did not carry the meaningful use stamp of approval, I would be the first to stand up and tell the world we should certify the dialysis information systems. Yet demonstrating such a benefit to patient care has proved remarkably elusive to date. In the absence of a benefit to patients, one thing is very clear, certifying our dialysis information systems will create substantial burdens for dialysis providers and nephrologists alike.
As the meaningful use program migrates from one in which providers are chasing positive incentives to one in which they are fleeing looming penalties and hoping they are not subject to an audit, I believe we will see nephrology provider behavior change. The proposed SGR fix is likely to create a new wrinkle in time, but I suspect it will require future rule making before the full impact is clear.



rg says
Terry,
In our practice, we are counting by provider. We are taking a 3 month period, and counting the number of office visits, and the number of dialysis visits. Each of the doctors are neck in neck (about 50 percent office—50 percent dialysis). That is because we do use a NP. We are hoping we can get the exclusion, but I cannot tell you until our 3 month trial is up on April 1. We do it by provider, not by group. So, Dr. G has 300 office, and Dr. G has 320 dialysis visits—he can then take the hardship, right? Or should we count by TOTAL GROUP: Entire group (not counting NP visits) has 600 office and 550 dialysis—The group can NOT take the hardship option. That is my question, would you suggest I count by group? Or, would you suggest I count by provider?
Terry Ketchersid, MD, MBA, VP, Clinical Health Information Management says
Good question RG. The MU program is measured and calculated at the individual provider level. In your example Dr G could in fact apply for the hardship exception, even if none of the other providers in the practice qualified for the exception. Of additional note, the hardship exceptions as written are examined on an annual basis, so if Dr G is successful this year, he or she would need to recalculate next year and submit an application for another hardship exception next year if the numbers lined up again.
Rafiq ElHammali says
In my practice I was able to show that my outpatient Dialysis rounds count for more than 50% of my outpatient visits, and planning to apply for the hardship.
Do we still have to attempt to log in to the CMS website and go through the attestation process even though that I know that I did not meet all the criteria, or should I go straight to the hardship application.
Terry Ketchersid, MD, MBA, VP, Clinical Health Information Management says
Good question Rafiq. The hardship exclusion and attesting from meaningful use are mutually exclusive choices, so if you file for the hardship exception and your exception is granted you would not need to log into the the CMS portal to attest from meaningful use.
PK says
Belated question–we can procrastinate with the best of them.
The providers in my practice fit scenario 2 above, with more than 50% of our face to face encounters are at the dialysis units. However, we are medical directors or have equity in at least some of the dialysis units, which are majority owned by the big two. The hardship exemption appears to require us to explain why we lack control over the decision to not employ CEHRT. Can you think of a good answer to this – as I don’t think our position will be unique here.
Terry Ketchersid, MD, MBA, VP, Clinical Health Information Management says
Great question and one many nephrologists encounter. The approach most are taking is to point out that absent either complete ownership, or a majority equity posotion in the facility, the decision to deploy CEHRT is outside of the nephrologists direct control. As the circumstance will vary by physician within your practice, the answers to this question need to recognize those unique circumstances. For example, the medical director in a nursing home does not control the decision to deploy CEHRT, the ownership of the nursing home controls that decision. Likewise, in the the vast majority of dialysis facility JVs, the dialysis organization is the majority partner by design. Ultimately it is the majority owner that controls the decision to deploy CEHRT.
PK says
I did not have enough encounters in 2012, 2013, 2014 and went to attest on the CMP website but couldn’t. I did not file for hardship. Is there anything I can do now? Thanks
PK says
Hi, I was unable to attest for 2012, 2013,2014 because of lack of output encounters(less than the required 50%). I was able to attest for 2011. I changed jobs in 2012. Each year we went to the cms website and were told I couldn’t attest.
I did not sign up for the hardship exemption though. Is there anything I can do now? Or am I doomed to take the 2% cut? Thanks
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Unfortunately PK, CMS has been very prescriptive about the window to file for a hardship exception. Historically, that window closes on July 1 of the year preceding the penalty year. For example, successfully attesting for MU during 2014 would permit you to avoid the 2% penalty in 2016. The other way to avoid the penalty would have been to successfully file a hardship exception prior to July 1, 2015. On a positive note, if you are unable to attest for MU this year, but you qualify for a hardship exception, you have until July 1, 2016 to file a hardship exception to avoid the 3% 2017 penalty