 Last week Dr. Dugan Maddux kindly gave us a reprieve from all of the MACRA talk on the blog. However, that break was short lived as we continue to unpackage the monster that is MIPS. With the first performance year being a short 6 months away—and no final ruling in sight—we want to keep you up to speed!
Last week Dr. Dugan Maddux kindly gave us a reprieve from all of the MACRA talk on the blog. However, that break was short lived as we continue to unpackage the monster that is MIPS. With the first performance year being a short 6 months away—and no final ruling in sight—we want to keep you up to speed!
So far we’ve covered 2 of the 4 MIPS categories (Quality and Advancing Care Information). Although the nomenclature has changed, these 2 categories are just our old friends PQRS and Meaningful Use with minor changes.
Another measurement activity
The biggest struggle over the past years has been keeping up with all the separate, complex CMS programs (such as MU, PQRS, and VM). Therefore, CMS combined everything into one program to help ease the reporting burden on clinicians. They also decided to remove measures and thresholds from the old MU/new ACI category and lower the amount of measures to be reported for the quality category. However, just when you thought you got the hang of things, out comes a whole new category—Clinical Practice Improvement Activities (CPIA).
 Figure 1: CPIA: The new piece of the MIPS puzzle
Figure 1: CPIA: The new piece of the MIPS puzzle
According to the MACRA proposed rule, CPIA is an activity that stakeholders identify as “improving clinical practice or care delivery and that the Secretary of HHS determines will likely result in improved outcomes.” The CPIA performance category also focuses on CMS’ strategic goals to use a “patient-centered approach to program development that leads to better, smarter, and healthier care.”
Unlike the other 3 MIPS categories, CPIA does not replace any current program and is a completely new concept brought to us by CMS. It is also a category with little detail and a lot of uncertainty.
CPIA will make up 15% of a clinician’s MIPS CPS (although this is subject to the Secretary’s authority to assign different scoring weights). Quite a hefty percentage for being the new kid on the block!
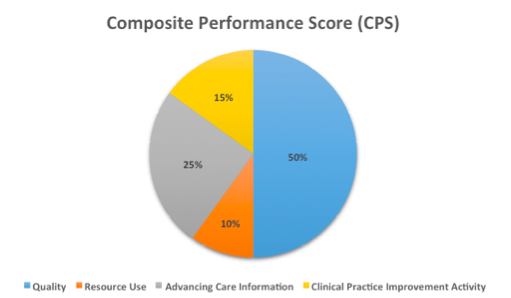
Figure 2: CPIA will comprise 15% of your total MIPS score
There are currently 90 activities listed in the proposed ruling. Each activity is assigned a subcategory (rings familiar to those National Quality Strategy (NQS) domains). Each activity is given a weight of either medium or high. CPIAs are weighted as high based on alignment with CMS national priorities and programs such as the Quality Innovation Network-Quality Improvement Organization (QIN/QIO) or the Comprehensive Primary Care Initiative or an activity identified as a public health priority (such as emphasis on anticoagulation management or utilization of prescription drug monitoring programs). The six proposed subcategories are shown below.
Some examples of high-weighted activities (20 points) include:
- Beneficiary Engagement: Collection and follow-up on patient experience and satisfaction data on beneficiary engagement, including development of improvement plan.
- Patient Safety and Practice Assessment: Consultation of Prescription Drug Monitoring Program prior to the issuance of a Controlled Substance Schedule II (CSII) opioid prescription that lasts for longer than 3 days.
Examples of medium-weighted activities (10 points) include:
- Care Coordination: Ensure that there is bilateral exchange of necessary patient information to guide patient care that could include one or more of the following: participate in a Health Information Exchange, if available, and/or use structured referral notes.
- Population Management: Participation in research that identifies interventions, tools, or processes that can improve a targeted patient population.
Initially, these activities must be conducted for a full 90 days during the performance year. A full list of proposed activities can be found on page 946 of the MACRA proposed rule.
Scoring
To achieve the highest score of 100 percent, an eligible clinician would need to attain 60 points and could do this by selecting and submitting data on a combination of activities. Activities that align with CMS national priorities and programs will be weighted as “high” and worth 20 points each; all others will be weighted as “medium” and worth 10 points each. Therefore, in order to receive the highest potential score (100 percent, or 60 points), clinicians will need to complete 3 high-weighted CPIAs or 6 medium-weighted CPIAs (or a combination thereof).
CMS did provide some exceptions to this category if a clinician meets one of the following:
- Part of a small group (consisting of 15 or fewer clinicians)
- Located in a rural area or geographic HPSAs
- Non-patient-facing
A clinician meeting any of the above criteria can achieve 100 percent by only reporting 2 activities, or can achieve 50 percent by reporting only 1 activity.
Advantage for medical homes and APMs
For some clinicians, this category will be a breeze, as they will automatically be given full or partial points without having to lift a finger. Clinicians that are a part of patient-centered medical home (PCMH) or participating in an APM will score favorably.
A clinician who is part of a “patient-centered medical home” or “comparable specialty practice” will automatically receive the full 60 points in this category. A patient-centered medical home is defined as a nationally recognized, accredited, patient-centered medical home, a Medicaid Medical Home Model, or a Medical Home Model. A comparable specialty practice must receive specialty-specific accreditation from the National Committee for Quality Assurance (NCQA).
Additionally, MIPS-eligible clinicians or groups who are participating in an alternative payment model (but do not qualify as an Advanced APM QP) will automatically receive 50 percent of the total CPIA score (30 points) just through their APM participation. This means they would only need an additional 30 points to reach the max score of 60 points.
For all other clinicians, you will start at ground zero and will need to reach 60 points through performing a combination of activities. It is obvious that the strategic goal from CMS is to drive movement toward delivery-system reform principles and APMs.
Lots of unknowns
There are still a lot of questions that need to be answered. In the first year, clinicians will have to identify which activities were selected and provide a “yes/no” attestation. However, CMS believes there should be a better way to measure and submit these activities (by examining clinical quality workflows and data capture and structure them similar to clinical quality measures).
CMS also makes it clear that the first year will be the “easiest” year for CPIA. They hope to create baseline requirements the first year and then build more stringent requirements in future years, laying the groundwork for expansion towards continuous improvement over time.
What do you think of this new category? We would like to hear your thoughts below!
 Diana Strubler, Senior Product Analyst, Health IT Standards, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.
Diana Strubler, Senior Product Analyst, Health IT Standards, joined Acumen in 2010 as an EHR trainer then quickly moved into the role of certification and health IT standards subject matter expert. She has successfully led Acumen through three certifications while also guiding our company and customers through the world of Meaningful Use, ICD-10 and PQRS.





Leave a Reply