October is well underway, leaves are changing colors, college football is off to a shaky start, and the sport of sports (college hoops) is just around the corner. Oh, yeah, and last week CMS finally got around to publishing the meaningful use final rule. That’s right, after six months and reportedly more than 2,500 public comments, the 752-page rule is ready for your review! Of course, there is far too much in this tome to cover in a single blog post, so today I thought we would hit a few of the high (and the low) points.
Reporting period
Perhaps the most anticipated piece of the puzzle is reporting period relief. CMS did not disappoint. As proposed, those of you planning to attest for 2015 may select any continuous 90-day period during calendar year 2015. Of course, it would have been nice to know this prior to the start of the fourth quarter; but this does indeed fall into that “better late than never” category. In addition, CMS has backtracked a bit in the final rule, and providers who are new to the MU program in 2016 and 2017 will also be granted the opportunity to attest for any continuous 90-day period during their first calendar year of participation. The rest of us will face the entire calendar year starting Jan. 1, 2016.
2015–2017
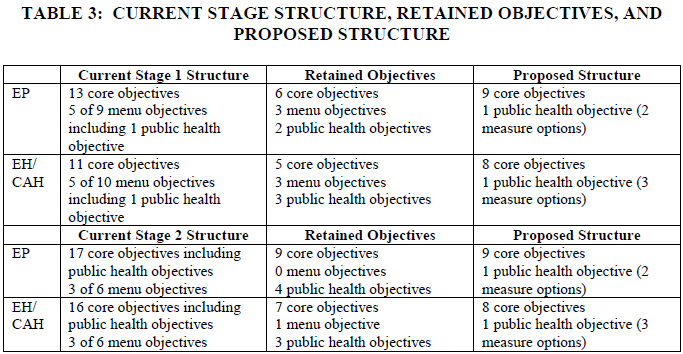
Additional big news in this final rule is a “dumbing-down” of the existing MU stages. In an apparent nod to the complexity of Stage 2 in particular, CMS has simplified Stages 1 and 2 for the remainder of their shelf lives. As noted in Table 3 below, CMS has done away with the core and menu framework and significantly reduced the number of objectives one must meet in each stage. Each of you lives in the “EP” or eligible professional bucket in the table below. Notice Stage 1 moves from 13 core and five menu objectives to 10 required objectives, and Stage 2 moves from 17 core and three menu to 10 required objectives.
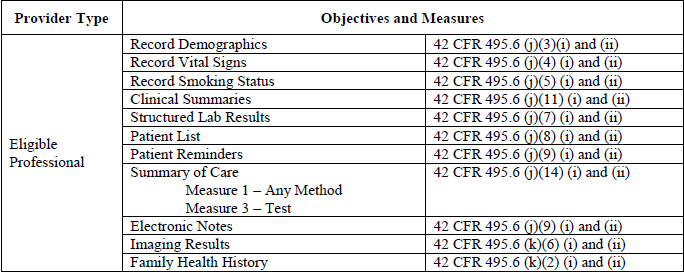
The devil as always is in the details, but in this case the details are favorable. CMS has very clearly heard the message-as-written. Not only is Stage 2 very difficult to achieve, but it is distracting us from delivering patient care. CMS arrives at the numbers in Table 3 by removing objectives that either are redundant or have “topped out.” Those measures that are riding off into the sunset are on display in the table below:
Stage 2
For those of you planning to participate in Stage 2 this year (CMS sure hopes there are a lot of you out there as participation to date has been very, very low), the 10 Stage 2 objectives you will face in 2015, 2016 and 2017 are:
- Protect PHI
- Clinical decision support
- CPOE
- eRx
- HIE (previously known as summary of care)
- Patient-specific education
- Medication reconciliation
- Patient eAccess to health information
- Secure messaging
- Public health/clinical data registry reporting
Even better than the smaller number of objectives is the recognition that the mechanics of several measures were remarkably difficult to achieve. There are too many examples to report in a single blog post, but the one that caught my attention is dropping the heavy requirements for patient participation as a requirement for your success. Measure 8 above now requires that a single patient view, download or transmit his or her health information during the reporting period, and Measure 9 only requires the provider attest to the fact that secure messaging was enabled during the reporting period. The actual exchange of messages between you and the patient is no longer required to clear the attestation hurdle.
Stage 3 delay?
Not so fast. In spite of the raucous chorus of requests to push Stage 3 out further, the final rule reads exactly as the proposed rule in this regard. All providers will be compelled to report Stage 3 in 2018. For those of you who wish to get a jump on things, you will have the option to report Stage 3 in 2017. They’ve also provided a carrot of sorts as those of you willing to start Stage 3 early will be afforded the luxury of a 90-day reporting period in 2017. If I were a betting man, I’d bet you will be able to count the number of nephrologists who select this option on one hand. By the way, this quirk in the reporting schedule will create all kinds of excitement for EHR vendors, vendors who would much rather devote resources to increasing usability and interoperability instead of racing the clock to be ready just in case a doc actually does want to dip his or her toe in the Stage 3 pond a year early. Makes one wonder what CMS/ONC was actually thinking by extending the option to participate in Stage 3 early. The “eight” proposed Stage 3 objectives remain largely intact and will almost certainly be the topic of a future post.
Is it really final?
One final point, in a bit of an odd twist, last week’s press release announced an additional 60-day comment period in order to “gather additional feedback about the EHR Incentive Programs going forward, in particular with the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), which established the Merit-based Incentive Payment System and consolidates certain aspects of a number of quality measurement and federal incentive programs into one more efficient framework. We will use this feedback to inform future policy developments for the EHR Incentive Programs, as well as consider it during rulemaking to implement MACRA, which we expect to release in the spring of 2016.” Final rule, indeed. Reading between the lines, one might wonder if we will see additional tweaks to the MU program before it’s all said and done.
Along those lines, take a close look at the meaningful use fact sheet published last week. This certainly does not read like the CMS fact sheets we have seen before. If I were a cynical nephrologist, I’d wonder if this was a veiled apology from the powers that be, perhaps a conciliatory note aimed at the massive groundswell of those calling for delays in the program. Notice how the authors proudly state that over 70 percent of eligible professionals have used a certified EHR. What’s missing is the embarrassingly low number of providers that attested last year, and what I suspect will be an even lower number this year. This fact sheet is also the first time I have seen CMS highlight and suggest the use of a hardship exception.
Over the next few weeks the Acumen team will be taking a deeper dive into the final rule. The good news? If you plan to play this year, you can indeed select any continuous 90-day period to report meaningful use. In addition, the Stage 2 lift is lighter this year than it was last year. Perhaps as importantly, you don’t have to worry about Stage 3 until 2018, the last year MU will exist as a stand-alone program. One final point is, with this announcement, CMS has let us know we will see detailed clarification of the MIPS program next spring. Clarity around MIPS will certainly be welcomed by the nephrology community.
Will you be attesting for meaningful use this year? Drop us a note and join the conversation.

Terry Ketchersid, MD, MBA, practiced nephrology for 15 years before spending the past seven years at Acumen focused on the Health IT needs of nephrologists. He currently holds the position of Chief Medical Officer for the Integrated Care Group at Fresenius Medical Care North America where he leverages his passion for Health IT to problem solve the coordination of care for the complex patient population served by the enterprise.




Bonnie Morgan says
We will certainly attest this year. We didn’t kill ourselves all year to meet these measures to not use them. We have met every measure except for those that are not available to us. My staff put a tremendous amount of work into meeting these measures.
Marc Falkowitz says
It appears most of your comments and rule changes are applying to stage two.
Our group is in second year, stage one. It happens that we have met all of the measures, however, it has been spread through the entire year. Can we still use the old time frame of one year for attestation purposes. Shrinking it to a 90 day window, at such a late date in the year, might make it near to impossible for us to comply.
thanks
Marc Falkowitz
Terry Ketchersid, MD, MBA, Chief Medical Officer - Integrated Care Group says
Hi Marc, the 90 day RP applies to everyone this year, stage 1 or Stage 2. I would bet your providers have several successful 90 day RPs logged this year. If not there is a lot of time left during the final 90 days of the month. Hope this helps.
Terry Ketchersid says
Actually Marc, a recent CMS FAQ has proven me wrong. During 2015 a provider may report any RP which lasts a minimum of 90 consecutive days but may include the full calendar year.Here is a link to that FAQ:
https://questions.cms.gov/faq.php?id=5005&faqId=12981
Best,
TK
Kathie Joseph says
We will be attesting this year. However, will start to look closely at the possibility of hardship.