 Thanksgiving has come and gone leaving behind a trail of football upsets and turkey day leftovers. The leftovers are one of my favorite parts of Thanksgiving. Whether it’s a late night turkey or ham sandwich, of perhaps the last slice of pecan pie, nothing beats the leftovers this time of year. Last week our blog welcomed Diana Strubler into our midst. Diana did a great job unpacking the quality reporting options available to nephrologists in 2015. As Diana pointed out, the 2015 physician fee schedule (PFS) final rule included over 1,000 double spaced pages. In the spirit of holiday leftovers, today we will explore another topic buried within that final rule—the 2015 updates for the physician value-based payment modifier, thankfully shortened to “the VM.”
Thanksgiving has come and gone leaving behind a trail of football upsets and turkey day leftovers. The leftovers are one of my favorite parts of Thanksgiving. Whether it’s a late night turkey or ham sandwich, of perhaps the last slice of pecan pie, nothing beats the leftovers this time of year. Last week our blog welcomed Diana Strubler into our midst. Diana did a great job unpacking the quality reporting options available to nephrologists in 2015. As Diana pointed out, the 2015 physician fee schedule (PFS) final rule included over 1,000 double spaced pages. In the spirit of holiday leftovers, today we will explore another topic buried within that final rule—the 2015 updates for the physician value-based payment modifier, thankfully shortened to “the VM.”
Who is in?
As with all of the CMS incentive programs, there is a bit of confusion about who is subject to the VM. As we described previously, the VM is measured and administered at the practice level, not the individual provider level. It is your practice’s Tax ID Number (TIN) that is under scrutiny within this CMS value-based purchasing program. There are over 1,300 practices in this country with more than 100 providers. Those practices are subject to the VM in 2015, based on the “value” their practice delivered in 2013.
The 2015 PFS final rule clarifies who is being measured in 2015 and beyond. Basically every practice that includes at least one provider on the list below is being measured in 2015:
- Doctors of medicine and osteopathy
- Doctors of dental surgery or dental medicine
- Doctors of podiatric medicine
- Doctors of optometry
- Chiropractors
Nephrologists are certainly on the hit parade, and regardless of practice size, next year every nephrology practice will be in the performance period for the 2017 VM adjustment. As noted below, those with 9 or fewer providers will not face “downside risk” in 2017, but they will be measured. What about practices participating in a Medicare Shared Savings program, like an ACO? Unlike previous VM years, for 2017 ACO participants will also be included in the VM. The final rule goes to great lengths to explain how this will happen, and for those of you involved with an ACO, I encourage you to review CMS’s plan for you and the VM.
Who is not?
Excluded from the 2017 VM are all non-physician eligible professionals. In 2013 CMS received a claim for services rendered from just over 1.25 million eligible professionals (EP) practicing in almost 300,000 groups around the country. Among the EPs are 908,000 physicians (see bulleted list above) and 360,000 non-physicians. Our NP and PA colleagues are included in the non-physician bucket, and while they are not part of the VM in 2017, they are included in 2018. Stated another way, in 2016 not only is the work done by your practice being measured, but the practice level VM applied in 2018 will impact payment for services delivered to Medicare beneficiaries by all of the providers in your medical practice.
Adjustments
As you may recall, during the 2015 performance period your practice’s performance will determine what “adjustment” the VM applies to your practice’s Medicare Part B allowable in 2017. That adjustment can either be a bonus, a penalty, or it can be neutral (0.0% in the tables below), meaning your practice will be paid according to the 2017 PFS. As part of its effort to ease practices into the program, during a practice’s first year of participation, CMS will hold the practice “harmless” with respect to the VM. In other words, during year one a practice will not incur a negative VM adjustment based on performance. This assumes however that your practice does not find itself in Category 2 defined below.
So, what does this mean for the 2015 performance period, which defines the 2017 VM adjustment? The answer depends on how many providers are in your practice. Table 88 from the final rule defines the 2017 VM payment adjustments for practices that have 9 or fewer providers:
Table 88. Final CY 2017 VM Payment Adjustment Amounts for Groups with Two to Nine Eligible Professionals and Solo Practitioners
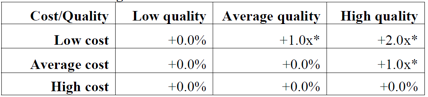
*Groups and solo practitioners eligible for an additional -1.0x if reporting measures and average beneficiary risk score is in the top 25 percent of all beneficiary risk scores, where “x” represents the upward payment adjustment factor.
Table 89 from the final rule highlights the 2017 VM adjustment for practices with 10 or more providers:
Table 89. Final CY 2017 VM Payment Adjustment Amounts for Groups with Ten or More Eligible Professionals
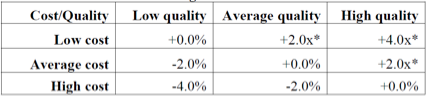
*Groups eligible for an additional -1.0x if reporting measures and average beneficiary risk score is in the top 25 percent of all beneficiary risk scores, where “x” represents the upward payment adjustment factor.
As previously reported in this blog, most providers are expected to fall into the neutral bucket (no penalty, no bonus), with a small percentage receiving a bonus and a small percentage facing a penalty. Remember, this is a budget-neutral program. The “bonus” paid to the practices the VM determines to be high performers is a function of the amount of money collected from those who are penalized. The “x” factor in the payment matrices above is determined by the amount of money collected from the poor performers.
Category 1 or 2?
Before we leave this subject for that last bite of pecan pie, let’s clarify one of the dirty little secrets of this program. Within the construct of the VM, one of the important components of your practice’s quality composite index is the performance of your physicians with respect to PQRS. Practices with providers who successfully participate in PQRS are put in a bucket labeled “category 1” and those who do not successfully report PQRS land in the bucket labeled “category 2.” If you do not successfully participate in PQRS, this creates a hole in the VM quality calculation. To discourage this, CMS will levy the maximum VM penalty upon practices in category 2. This is clearly defined in the 2015 PFS final rule. In other words, if less than 50% of the providers in your practice successfully report PQRS in 2015, the practice’s VM adjustment will be the maximum penalty (2% for practices with 9 or fewer providers and 4% for every other practice). Note this penalty is additive to the 2% penalty each provider will incur for not successfully reporting PQRS in 2015. Bottom line, fail to report PQRS in 2015 and you will likely face a 4% or 6% reduction in your 2017 Medicare PFS. Now that’s a leftover no one will want to taste!




rg says
Great post. Put a fork in me, I’m done. We are in an ACA, but have fewer than 9 providers. Does that me we are on the hook for the possible penalty? The way I read your post is that because this is the 1st year of participation, we cannot get a penalty. Also, are they defining quality based on the 6 measures for PQRS that our colleague posted last week—or is the complexity of the ACA that you refer to above? Are we still in the “harmless category,” or are we in category two now? The way I read it is that we are still in category one, correct? I don’t want to be a turkey next year and get the penalty.
Terry Ketchersid, MD, MBA, VP, Clinical Health Information Management says
Very good question RG. You will be held harmless unless 5 of your docs (more than 50% of your providers) do not report PQRS successfully in 2015, in which case they will park your practice in Category 2 and extend the maximum VM prenalty to your practice in 2017.